Open Access
Review
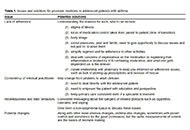
Precision medicine: how to approach the adolescent asthmatic
Alan Kaplan
Published: October 31, 2023 Explor Asthma Allergy. 2023;1:153–162
This article belongs to the special issue Precision Medicine in Allergy and Rhinology
Open Access
Correction
Correction: Omega-5-gliadin-specific immunoglobulin E-positive, but wheat-specific immunoglobulin E-negative wheat allergy dependent on augmentation factors—a frequent presentation
Editorial Office
Published: January 17, 2024 Explor Asthma Allergy. 2024;2:1
Open Access
Consensus Statement
Manifesto of the rights and duties of persons with respiratory allergies
Mario Di Gioacchino ... Giorgio Walter Canonica
Published: February 07, 2025 Explor Asthma Allergy. 2025;3:100972
Open Access
Review
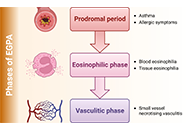
New therapeutic approaches with biological drugs for eosinophilic granulomatosis with polyangiitis
Alejandra Carrón-Herrero ... Giovanni Paoletti
Published: June 08, 2023 Explor Asthma Allergy. 2023;1:31–48
This article belongs to the special issue The Era of Biologics in Allergy
Open Access
Original Article
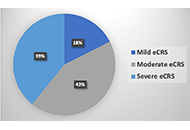
Assessing chronic rhinosinusitis with nasal polyps severity by “Japanese epidemiological survey of refractory eosinophilic chronic rhinosinusitis” algorithm
Sérgio Duarte Dortas ... Solange Oliveira Rodrigues Valle
Published: June 16, 2023 Explor Asthma Allergy. 2023;1:49–54
This article belongs to the special issue Precision Medicine in Allergy and Rhinology
Open Access
Case Report
Food fish allergy as a result of occupational exposure to fish collagen
Felipe Santos Vicente ... Borja Bartolomé Zavala
Published: June 30, 2023 Explor Asthma Allergy. 2023;1:55–59
Open Access
Review
Eosinophilic gastrointestinal disorders: new perspectives and the emerging role of biological therapies
Francesca Losa, Arianna Cingolani
Published: June 30, 2023 Explor Asthma Allergy. 2023;1:60–72
This article belongs to the special issue The Era of Biologics in Allergy

Open Access
Review
Small airway dysfunction and obesity in asthmatic patients: a dangerous liaison?
Jack Pepys ... Marcello Cottini
Published: August 15, 2023 Explor Asthma Allergy. 2023;1:73–88
Open Access
Review
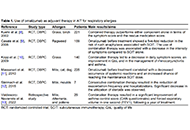
Can we apply biomarkers in the management of non-steroidal anti-inflammatory drug exacerbated respiratory disease?
Hyo-In Rhyou ... Hae-Sim Park
Published: August 24, 2023 Explor Asthma Allergy. 2023;1:89–106

Open Access
Letter to the Editor
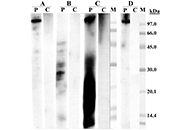
Impact of the standardization unit’s definition on the in vitro biological potency of allergen extracts
Thierry Batard ... Laurent Mascarell
Published: August 27, 2023 Explor Asthma Allergy. 2023;1:107–114

Open Access
Review
Impact of the GINA asthma guidelines 2019 revolution on local asthma guidelines and challenges: special attention to the GCC countries
Riyad Allehebi, Hamdan AL-Jahdali
Published: October 10, 2023 Explor Asthma Allergy. 2023;1:115–125
This article belongs to the special issue The Global Picture of Asthma after Guideline Changes and the COVID Pandemics
Open Access
Review
Biologic drugs and allergen immunotherapy: potential allies
Palma Carlucci ... Danilo Di Bona
Published: October 20, 2023 Explor Asthma Allergy. 2023;1:126–141
This article belongs to the special issue The Era of Biologics in Allergy

Open Access
Editorial
Exploration of Asthma & Allergy, where science, evidence, and vision can improve clinical practice
Giorgio Walter Canonica, Enrico Heffler
Published: March 01, 2023 Explor Asthma Allergy. 2023;1:1–3
Open Access
Mini Review
TSLP and asthma: fellow travelers
David El-Qutob, Antonio Letran
Published: April 14, 2023 Explor Asthma Allergy. 2023;1:4–10
Open Access
Original Article
An exploratory study on the validity and reliability of the Greek translation of Juniper’s Asthma Control Questionnaire in pediatric patients in Greece
Maria M. Papamichael ... Bircan Erbas
Published: April 23, 2023 Explor Asthma Allergy. 2023;1:11–19

Open Access
Case Report
Isolated lettuce allergy in a medical student: case report and review of the literature
Kyle Alexander ... Nicolaos Nicolaou
Published: April 26, 2023 Explor Asthma Allergy. 2023;1:20–27
Open Access
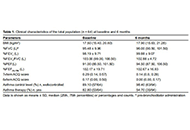
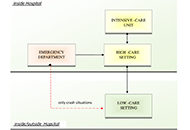
Letter to the Editor
Allergists/immunologists facing the coronavirus disease 2019 pandemic: the experience of managing a low-care setting
Laura Franceschini ... Alessandro Farsi
Published: April 27, 2023 Explor Asthma Allergy. 2023;1:28–30
Open Access
Original Article
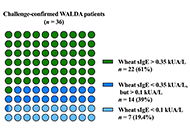
Omega-5-gliadin-specific immunoglobulin E-positive, but wheat-specific immunoglobulin E-negative wheat allergy dependent on augmentation factors—a frequent presentation
Valentina Faihs ... Knut Brockow
Published: December 28, 2023 Explor Asthma Allergy. 2023;1:230–238
This article belongs to the special issue The Different Faces of Food Allergy

Open Access
Case Report
Clinical responses and relapses in omalizumab-assisted desensitization to food in children: long-term evolution in real life
Angel Mazon ... Antonio Nieto
Published: January 30, 2024 Explor Asthma Allergy. 2024;2:2–8
This article belongs to the special issue The Different Faces of Food Allergy

Open Access
Review
Management of asthma using probiotics
Amar P. Garg ... Bajeerao Patil
Published: February 20, 2024 Explor Asthma Allergy. 2024;2:9–32
This article belongs to the special issue Asthma and its Relationship with Psychological and Psychopathological Factors

