The impact of occupational exposures on chronic rhinosinusitis: a scoping review
Chronic rhinosinusitis (CRS) is a prevalent and burdensome condition worldwide, characterized by inflammation of the paranasal sinuses. Ideally, instead of treating CRS, we would identify ways to pr
[...] Read more.
Chronic rhinosinusitis (CRS) is a prevalent and burdensome condition worldwide, characterized by inflammation of the paranasal sinuses. Ideally, instead of treating CRS, we would identify ways to prevent the development of this chronic condition. Occupational exposures may be an excellent target for prevention. Occupational exposures have been shown to play a critical role in the pathogenesis of multiple lower airway diseases, such as asthma, silicosis, asbestosis, and hypersensitivity pneumonitis. However, evidence for the association between occupational exposures and the development of upper airway disease, like CRS, is less well-defined. This manuscript examines the association between occupational exposures and CRS. A scoping review of the literature following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines identified 19 relevant studies. The populations examined and the methods and criteria used for defining CRS diagnosis and occupational variables significantly varied between the studies. Diagnosis of CRS was most often determined by self-reported symptoms or medical record review. Occupational variables ranged from employment status to occupation type to specific exogenous compounds encountered. Overall, substantial evidence demonstrates a general association between occupational exposures and CRS diagnosis; however, limitations in study methodologies, including variations in CRS diagnostic criteria, occupational exposures, assessment methods, and populations, hinder drawing more specific conclusions. Moving forward, rigorous research methodologies and standardized criteria are essential to draw conclusions supported by multiple studies. Critical components of future studies should include large, diverse populations, use of consensus CRS diagnostic criteria, and inclusion of many specific and quantitatively defined exposures. Ultimately, such efforts can help inform preventative measures and interventions for CRS, thus mitigating the burden of CRS on individuals and populations worldwide.
Aurelia S. Monk ... Adam J. Kimple
View:598
Download:16
Times Cited: 0
Chronic rhinosinusitis (CRS) is a prevalent and burdensome condition worldwide, characterized by inflammation of the paranasal sinuses. Ideally, instead of treating CRS, we would identify ways to prevent the development of this chronic condition. Occupational exposures may be an excellent target for prevention. Occupational exposures have been shown to play a critical role in the pathogenesis of multiple lower airway diseases, such as asthma, silicosis, asbestosis, and hypersensitivity pneumonitis. However, evidence for the association between occupational exposures and the development of upper airway disease, like CRS, is less well-defined. This manuscript examines the association between occupational exposures and CRS. A scoping review of the literature following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines identified 19 relevant studies. The populations examined and the methods and criteria used for defining CRS diagnosis and occupational variables significantly varied between the studies. Diagnosis of CRS was most often determined by self-reported symptoms or medical record review. Occupational variables ranged from employment status to occupation type to specific exogenous compounds encountered. Overall, substantial evidence demonstrates a general association between occupational exposures and CRS diagnosis; however, limitations in study methodologies, including variations in CRS diagnostic criteria, occupational exposures, assessment methods, and populations, hinder drawing more specific conclusions. Moving forward, rigorous research methodologies and standardized criteria are essential to draw conclusions supported by multiple studies. Critical components of future studies should include large, diverse populations, use of consensus CRS diagnostic criteria, and inclusion of many specific and quantitatively defined exposures. Ultimately, such efforts can help inform preventative measures and interventions for CRS, thus mitigating the burden of CRS on individuals and populations worldwide.
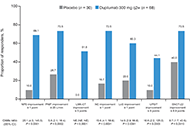 Dupilumab improved objective and patient-reported outcomes in patients with chronic rhinosinusitis with nasal polyps and complete nasal obstructionOpen AccessOriginal ArticleAim: The impact of complete bilateral nasal obstruction [nasal polyp score (NPS) = 8/8] on treatment outcomes in chronic rhinosinusitis with nasal polyps (CRSwNP) is unclear. This post hoc analys [...] Read more.Martin Wagenmann ... Juby A. Jacob-NaraPublished: July 30, 2024 Explor Asthma Allergy. 2024;2:363–372
Dupilumab improved objective and patient-reported outcomes in patients with chronic rhinosinusitis with nasal polyps and complete nasal obstructionOpen AccessOriginal ArticleAim: The impact of complete bilateral nasal obstruction [nasal polyp score (NPS) = 8/8] on treatment outcomes in chronic rhinosinusitis with nasal polyps (CRSwNP) is unclear. This post hoc analys [...] Read more.Martin Wagenmann ... Juby A. Jacob-NaraPublished: July 30, 2024 Explor Asthma Allergy. 2024;2:363–372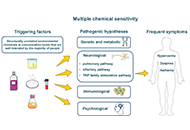 Multiple chemical sensitivity: a review of its pathophysiologyOpen AccessReviewMultiple chemical sensitivity (MCS) is an unexplained acquired medical condition that includes multiple, vague, recurrent, and non-specific symptoms in different organs. They are attributed to expos [...] Read more.Cătălina Elena Lavric ... Frédéric de BlayPublished: July 29, 2024 Explor Asthma Allergy. 2024;2:350–362
Multiple chemical sensitivity: a review of its pathophysiologyOpen AccessReviewMultiple chemical sensitivity (MCS) is an unexplained acquired medical condition that includes multiple, vague, recurrent, and non-specific symptoms in different organs. They are attributed to expos [...] Read more.Cătălina Elena Lavric ... Frédéric de BlayPublished: July 29, 2024 Explor Asthma Allergy. 2024;2:350–362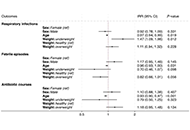 Impact of reduced COVID-19 restrictions on pediatric recurrent respiratory infections in Southern Italy: a cross-sectional analysisOpen AccessOriginal ArticleAim: This study investigated changes in pediatric respiratory health resulting from the easing of COVID-19-related social restrictions, following a noted decrease in respiratory infections during [...] Read more.Cristiana Indolfi ... Michele Miraglia del GiudicePublished: July 24, 2024 Explor Asthma Allergy. 2024;2:340–349
Impact of reduced COVID-19 restrictions on pediatric recurrent respiratory infections in Southern Italy: a cross-sectional analysisOpen AccessOriginal ArticleAim: This study investigated changes in pediatric respiratory health resulting from the easing of COVID-19-related social restrictions, following a noted decrease in respiratory infections during [...] Read more.Cristiana Indolfi ... Michele Miraglia del GiudicePublished: July 24, 2024 Explor Asthma Allergy. 2024;2:340–349 The search for still unknown pathomechanisms of allergyOpen AccessReviewIn recent decades, atopic diseases, such as atopic dermatitis (AD), allergic asthma (AA), allergic rhinitis (AR), and food allergy (FA) have been estimated rapidly increasing in prevalence. These di [...] Read more.Gualtiero Leo ... Stefania ArasiPublished: July 22, 2024 Explor Asthma Allergy. 2024;2:329–339
The search for still unknown pathomechanisms of allergyOpen AccessReviewIn recent decades, atopic diseases, such as atopic dermatitis (AD), allergic asthma (AA), allergic rhinitis (AR), and food allergy (FA) have been estimated rapidly increasing in prevalence. These di [...] Read more.Gualtiero Leo ... Stefania ArasiPublished: July 22, 2024 Explor Asthma Allergy. 2024;2:329–339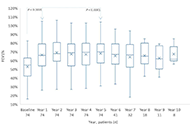 Long-term evaluation of omalizumab therapy in patients with severe allergic asthmaOpen AccessOriginal ArticleAim: Evaluation of real-world data regarding the use of omalizumab on lung function, asthma control, exacerbations, and oral corticosteroid (OCS). Methods: The single-centre, retrospective [...] Read more.Karl-Christian Bergmann ... Torsten ZuberbierPublished: July 19, 2024 Explor Asthma Allergy. 2024;2:319–328
Long-term evaluation of omalizumab therapy in patients with severe allergic asthmaOpen AccessOriginal ArticleAim: Evaluation of real-world data regarding the use of omalizumab on lung function, asthma control, exacerbations, and oral corticosteroid (OCS). Methods: The single-centre, retrospective [...] Read more.Karl-Christian Bergmann ... Torsten ZuberbierPublished: July 19, 2024 Explor Asthma Allergy. 2024;2:319–328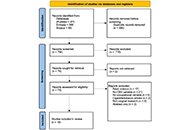 The impact of occupational exposures on chronic rhinosinusitis: a scoping reviewOpen AccessReviewChronic rhinosinusitis (CRS) is a prevalent and burdensome condition worldwide, characterized by inflammation of the paranasal sinuses. Ideally, instead of treating CRS, we would identify ways to pr [...] Read more.Aurelia S. Monk ... Adam J. KimplePublished: July 19, 2024 Explor Asthma Allergy. 2024;2:301–318
The impact of occupational exposures on chronic rhinosinusitis: a scoping reviewOpen AccessReviewChronic rhinosinusitis (CRS) is a prevalent and burdensome condition worldwide, characterized by inflammation of the paranasal sinuses. Ideally, instead of treating CRS, we would identify ways to pr [...] Read more.Aurelia S. Monk ... Adam J. KimplePublished: July 19, 2024 Explor Asthma Allergy. 2024;2:301–318 A treatable traits approach for asthma in a post-COVID eraOpen AccessReviewAs a novel respiratory viral infection, coronavirus disease 2019 (COVID-19) has influenced asthma in unpredictable ways. In the post-COVID era, there is a need to review asthma care and the new chal [...] Read more.Yuto Hamada ... Peter Gerard GibsonPublished: June 27, 2024 Explor Asthma Allergy. 2024;2:287–300
A treatable traits approach for asthma in a post-COVID eraOpen AccessReviewAs a novel respiratory viral infection, coronavirus disease 2019 (COVID-19) has influenced asthma in unpredictable ways. In the post-COVID era, there is a need to review asthma care and the new chal [...] Read more.Yuto Hamada ... Peter Gerard GibsonPublished: June 27, 2024 Explor Asthma Allergy. 2024;2:287–300