Rheumatoid arthritis: a complex tale of autoimmune hypersensitivity
Rheumatoid arthritis (RA) is a complex autoimmune disorder characterized by a spectrum of hypersensitivity reactions, encompassing Type II, Type III, and Type IV responses. Firstly, RA is marked by
[...] Read more.
Rheumatoid arthritis (RA) is a complex autoimmune disorder characterized by a spectrum of hypersensitivity reactions, encompassing Type II, Type III, and Type IV responses. Firstly, RA is marked by Type II hypersensitivity reactions driven by autoantibodies, such as rheumatoid factor (RF) and anti-(cyclic) citrullinated protein antibodies (ACPAs). These autoantibodies serve not only as serological markers for RA but also actively participate in inflammation, bone erosion, and clinical outcomes, with concurrent activation of the complement system involving C1q, C3, and C5 components specifically linked to RA progression and bone damage. Secondly, RA exhibits traits of Type III hypersensitivity, marked by the formation of immune complexes inciting inflammatory reactions. Immunoglobulin G (IgG) autoantibodies like RF and ACPA play pivotal roles in immune complex formation and the ensuing inflammatory responses. RA also demonstrates Type IV hypersensitivity propelled by CD4+ T cells, encompassing T helper 1 (Th1) and Th17 subsets. Th1 cells release interferon (IFN)-γ, promoting proinflammatory cytokines, while Th17 cells secrete IL-17, IL-22, and granulocyte-macrophage colony-stimulating factor (GM-CSF), contributing to synovial inflammation, bone and cartilage damage, and angiogenesis. RA concurrently exhibits features of Type II, Type III, and Type IV hypersensitivity. It is crucial to comprehend the presence and complex interplay of hypersensitivity responses and specific immune cell subsets in RA to create precise and efficient therapeutic approaches for the management of this incapacitating autoimmune condition. Thus, in this review, we aim to provide a comprehensive overview of the hypersensitivity features of RA.
Jihye Heo ... Jea-Hyun Baek
View:4504
Download:60
Times Cited: 0
Rheumatoid arthritis (RA) is a complex autoimmune disorder characterized by a spectrum of hypersensitivity reactions, encompassing Type II, Type III, and Type IV responses. Firstly, RA is marked by Type II hypersensitivity reactions driven by autoantibodies, such as rheumatoid factor (RF) and anti-(cyclic) citrullinated protein antibodies (ACPAs). These autoantibodies serve not only as serological markers for RA but also actively participate in inflammation, bone erosion, and clinical outcomes, with concurrent activation of the complement system involving C1q, C3, and C5 components specifically linked to RA progression and bone damage. Secondly, RA exhibits traits of Type III hypersensitivity, marked by the formation of immune complexes inciting inflammatory reactions. Immunoglobulin G (IgG) autoantibodies like RF and ACPA play pivotal roles in immune complex formation and the ensuing inflammatory responses. RA also demonstrates Type IV hypersensitivity propelled by CD4+ T cells, encompassing T helper 1 (Th1) and Th17 subsets. Th1 cells release interferon (IFN)-γ, promoting proinflammatory cytokines, while Th17 cells secrete IL-17, IL-22, and granulocyte-macrophage colony-stimulating factor (GM-CSF), contributing to synovial inflammation, bone and cartilage damage, and angiogenesis. RA concurrently exhibits features of Type II, Type III, and Type IV hypersensitivity. It is crucial to comprehend the presence and complex interplay of hypersensitivity responses and specific immune cell subsets in RA to create precise and efficient therapeutic approaches for the management of this incapacitating autoimmune condition. Thus, in this review, we aim to provide a comprehensive overview of the hypersensitivity features of RA.
 Herpes simplex virus-mediated skin infections: cytokines and its interplayOpen AccessReviewThe skin, as the first physical barrier for invading pathogens, also serves as an immunologically active organ. Breaching the skin barrier is thus essential for pathogens to enter the body. The skin [...] Read more.Aparna Mukhopadhyay ... Debprasad ChattopadhyayPublished: June 30, 2024 Explor Immunol. 2024;4:394–413
Herpes simplex virus-mediated skin infections: cytokines and its interplayOpen AccessReviewThe skin, as the first physical barrier for invading pathogens, also serves as an immunologically active organ. Breaching the skin barrier is thus essential for pathogens to enter the body. The skin [...] Read more.Aparna Mukhopadhyay ... Debprasad ChattopadhyayPublished: June 30, 2024 Explor Immunol. 2024;4:394–413 Dengue virus infection induces complement factor H but protein remains cell-associated, with changes intracellularly and in cell surface bindingOpen AccessOriginal ArticleAim: Severe dengue is correlated with a decrease in the circulating complement regulator, factor H (FH) and prior work has shown that dengue virus (DENV) infection induces FH mRNA but not FH prot [...] Read more.Joshua G. Dubowsky ... Jillian M. CarrPublished: June 24, 2024 Explor Immunol. 2024;4:376–393
Dengue virus infection induces complement factor H but protein remains cell-associated, with changes intracellularly and in cell surface bindingOpen AccessOriginal ArticleAim: Severe dengue is correlated with a decrease in the circulating complement regulator, factor H (FH) and prior work has shown that dengue virus (DENV) infection induces FH mRNA but not FH prot [...] Read more.Joshua G. Dubowsky ... Jillian M. CarrPublished: June 24, 2024 Explor Immunol. 2024;4:376–393 Rheumatoid arthritis: a complex tale of autoimmune hypersensitivityOpen AccessReviewRheumatoid arthritis (RA) is a complex autoimmune disorder characterized by a spectrum of hypersensitivity reactions, encompassing Type II, Type III, and Type IV responses. Firstly, RA is marked by [...] Read more.Jihye Heo ... Jea-Hyun BaekPublished: June 20, 2024 Explor Immunol. 2024;4:358–375
Rheumatoid arthritis: a complex tale of autoimmune hypersensitivityOpen AccessReviewRheumatoid arthritis (RA) is a complex autoimmune disorder characterized by a spectrum of hypersensitivity reactions, encompassing Type II, Type III, and Type IV responses. Firstly, RA is marked by [...] Read more.Jihye Heo ... Jea-Hyun BaekPublished: June 20, 2024 Explor Immunol. 2024;4:358–375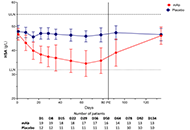 Safety and tolerability of anti-FcRn monoclonal antibody in thyroid autoimmunityOpen AccessOriginal ArticleAim: The clinical symptoms of autoantibody (AAb)-mediated autoimmune diseases (AID) usually correlate with the AAb-titer. Immunoglobulins (Igs) of the IgG type are actively recycled by the neonat [...] Read more.Jan Wolf ... George J. KahalyPublished: June 20, 2024 Explor Immunol. 2024;4:341–357
Safety and tolerability of anti-FcRn monoclonal antibody in thyroid autoimmunityOpen AccessOriginal ArticleAim: The clinical symptoms of autoantibody (AAb)-mediated autoimmune diseases (AID) usually correlate with the AAb-titer. Immunoglobulins (Igs) of the IgG type are actively recycled by the neonat [...] Read more.Jan Wolf ... George J. KahalyPublished: June 20, 2024 Explor Immunol. 2024;4:341–357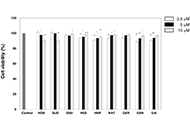 Flavonoids, nobiletin, heptamethoxyflavone, and genistein enhance antigen-presenting cell function in vitroOpen AccessOriginal ArticleAim: Antigen (Ag) presentation by Ag-presenting cells (APCs) is the first step in the generation of adaptive humoral and cellular immune responses. However, there have been few studies on the eff [...] Read more.Yuko Tanaka ... Tohru SakaiPublished: May 29, 2024 Explor Immunol. 2024;4:333–340
Flavonoids, nobiletin, heptamethoxyflavone, and genistein enhance antigen-presenting cell function in vitroOpen AccessOriginal ArticleAim: Antigen (Ag) presentation by Ag-presenting cells (APCs) is the first step in the generation of adaptive humoral and cellular immune responses. However, there have been few studies on the eff [...] Read more.Yuko Tanaka ... Tohru SakaiPublished: May 29, 2024 Explor Immunol. 2024;4:333–340 The immune response of nano carbon-based photic-driving vaccines to severe acute respiratory syndrome coronavirus 2Open AccessPerspectiveAs the most severe novel infectious disease in this century, coronavirus disease 2019 (COVID-19) faces tremendous challenges due to the hysteresis of drugs and vaccine development. Elucidating the p [...] Read more.Junming Chen ... Jianshe YangPublished: May 17, 2024 Explor Immunol. 2024;4:325–332
The immune response of nano carbon-based photic-driving vaccines to severe acute respiratory syndrome coronavirus 2Open AccessPerspectiveAs the most severe novel infectious disease in this century, coronavirus disease 2019 (COVID-19) faces tremendous challenges due to the hysteresis of drugs and vaccine development. Elucidating the p [...] Read more.Junming Chen ... Jianshe YangPublished: May 17, 2024 Explor Immunol. 2024;4:325–332 Recent advances in the study of the structure and function of the epididymisOpen AccessReviewTesticular sperm maturation is critical for establishing male fertility. Spermatozoa undergo remodeling of sperm proteins and changes in lipid and ribonucleic acid composition during transport in th [...] Read more.Chuxiong Wang ... Donghui HuangPublished: May 17, 2024 Explor Immunol. 2024;4:309–324
Recent advances in the study of the structure and function of the epididymisOpen AccessReviewTesticular sperm maturation is critical for establishing male fertility. Spermatozoa undergo remodeling of sperm proteins and changes in lipid and ribonucleic acid composition during transport in th [...] Read more.Chuxiong Wang ... Donghui HuangPublished: May 17, 2024 Explor Immunol. 2024;4:309–324