Metabolic correction of neurodegenerative pathologies: the role of macronutrients and timing
Despite decades of intensive research, effective treatment and prevention strategies for neurodegenerative diseases (NDDs) remain elusive. This review focuses on Alzheimer’s and Parkinson’s dise
[...] Read more.
Despite decades of intensive research, effective treatment and prevention strategies for neurodegenerative diseases (NDDs) remain elusive. This review focuses on Alzheimer’s and Parkinson’s diseases and acquired epilepsy suggesting that in their early phase, these progressive pathologies share common or interacting molecular pathways. Indeed, oxidative stress associated with disrupted glucose metabolism is the expected end state of most, if not all, risk factors preceding the onset of major NDDs. This review proposes that the initial oxidative stress in the brain resulting specifically from the hyperactivation of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX) causes a decline in glucose utilization and is the primary initiating factor of major NDDs. The existing clinical and experimental evidence points to NOX as the primary initiating mechanism shared within the major NDDs. During early oxidative stress, NOX activation is triggered in variable brain cells via multiple pathways, from beta-amyloid to alpha-synuclein, fibrin to glutamate and seizures. Therefore, the treatment strategy should have targeted the activation of NOX, wouldn’t there be a lack of clinically approved selective NOX antagonists? On the other hand, there are promising metabolism-altering approaches via dietary means able to switch energy intake from glucose to ketones, which influences both oxidative stress and glucose utilization and could ameliorate disease progression. The regimen of time-restricted eating appears to be the most feasible, nutritious, and palatable one providing the essential benefits of a ketogenic diet without adverse effects.
Yuri Zilberter, Tanya Zilberter
View:3166
Download:55
Times Cited: 0
Despite decades of intensive research, effective treatment and prevention strategies for neurodegenerative diseases (NDDs) remain elusive. This review focuses on Alzheimer’s and Parkinson’s diseases and acquired epilepsy suggesting that in their early phase, these progressive pathologies share common or interacting molecular pathways. Indeed, oxidative stress associated with disrupted glucose metabolism is the expected end state of most, if not all, risk factors preceding the onset of major NDDs. This review proposes that the initial oxidative stress in the brain resulting specifically from the hyperactivation of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase (NOX) causes a decline in glucose utilization and is the primary initiating factor of major NDDs. The existing clinical and experimental evidence points to NOX as the primary initiating mechanism shared within the major NDDs. During early oxidative stress, NOX activation is triggered in variable brain cells via multiple pathways, from beta-amyloid to alpha-synuclein, fibrin to glutamate and seizures. Therefore, the treatment strategy should have targeted the activation of NOX, wouldn’t there be a lack of clinically approved selective NOX antagonists? On the other hand, there are promising metabolism-altering approaches via dietary means able to switch energy intake from glucose to ketones, which influences both oxidative stress and glucose utilization and could ameliorate disease progression. The regimen of time-restricted eating appears to be the most feasible, nutritious, and palatable one providing the essential benefits of a ketogenic diet without adverse effects.
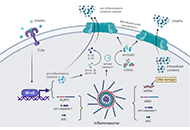 Inflammatory responses involved in post-cardiac arrest brain injury: mechanisms, regulation, and therapeutic potentialOpen AccessReviewNeuroinflammation plays a key role in the pathogenesis of post-cardiac arrest (CA) brain injury. Innate immune cells sense a variety of danger signals through pattern-recognition receptors and evoke [...] Read more.Yuzhen Zhang ... Kaibin HuangPublished: April 26, 2023 Explor Neurosci. 2023;2:82–97
Inflammatory responses involved in post-cardiac arrest brain injury: mechanisms, regulation, and therapeutic potentialOpen AccessReviewNeuroinflammation plays a key role in the pathogenesis of post-cardiac arrest (CA) brain injury. Innate immune cells sense a variety of danger signals through pattern-recognition receptors and evoke [...] Read more.Yuzhen Zhang ... Kaibin HuangPublished: April 26, 2023 Explor Neurosci. 2023;2:82–97 Metabolic correction of neurodegenerative pathologies: the role of macronutrients and timingOpen AccessReviewDespite decades of intensive research, effective treatment and prevention strategies for neurodegenerative diseases (NDDs) remain elusive. This review focuses on Alzheimer’s and Parkinson’s dise [...] Read more.Yuri Zilberter, Tanya ZilberterPublished: April 21, 2023 Explor Neurosci. 2023;2:67–81
Metabolic correction of neurodegenerative pathologies: the role of macronutrients and timingOpen AccessReviewDespite decades of intensive research, effective treatment and prevention strategies for neurodegenerative diseases (NDDs) remain elusive. This review focuses on Alzheimer’s and Parkinson’s dise [...] Read more.Yuri Zilberter, Tanya ZilberterPublished: April 21, 2023 Explor Neurosci. 2023;2:67–81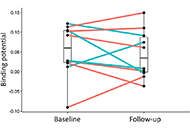 The effect of the tumour necrosis factor-alpha-inhibitor etanercept on microglial activation patients with mild cognitive impairment—a PET studyOpen AccessOriginal ArticleAim: Microglial activation is increasingly recognised as a factor in the progression of Alzheimer’s disease (AD) and may be modified by systemic inflammatory signals including serum tumour necrosis factor (TNF)-α. The aim was t [...] Read more.Alexander Gerhard ... Clive HolmesPublished: March 26, 2023 Explor Neurosci. 2023;2:52–66
The effect of the tumour necrosis factor-alpha-inhibitor etanercept on microglial activation patients with mild cognitive impairment—a PET studyOpen AccessOriginal ArticleAim: Microglial activation is increasingly recognised as a factor in the progression of Alzheimer’s disease (AD) and may be modified by systemic inflammatory signals including serum tumour necrosis factor (TNF)-α. The aim was t [...] Read more.Alexander Gerhard ... Clive HolmesPublished: March 26, 2023 Explor Neurosci. 2023;2:52–66