Open Access
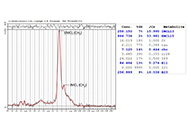
Original Article
Utility of dimethylsulfoxide to preserve synovial fluid samples for microcrystal detection and identification
Fernando Pérez-Ruiz ... Juan J. Mateos-Mazón
Published: February 21, 2023 Explor Musculoskeletal Dis. 2023;1:4–10
Open Access
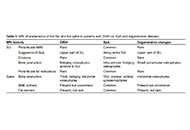
Case Report
Similarities and differences between gouty arthritis and rheumatoid arthritis—an interesting case with a short look into the literature
David Kiefer ... Juergen Braun
Published: February 24, 2023 Explor Musculoskeletal Dis. 2023;1:11–19

Open Access
Perspective
Towards a more ambitious uricemia target to improve joint and cardiovascular outcomes in gout
Enrique Calvo-Aranda, Fernando Perez-Ruiz
Published: February 27, 2023 Explor Musculoskeletal Dis. 2023;1:20–25
Open Access
Original Article
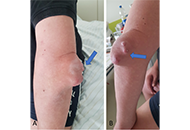
Infection after reconstruction of the anterior cruciate ligament
Elisha Krasin ... Yaniv Warschawski
Published: February 27, 2023 Explor Musculoskeletal Dis. 2023;1:26–30
Open Access
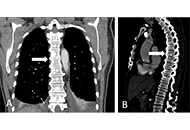
Case Report
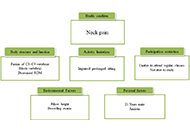
Physiotherapy management of a patient with neck pain having block vertebra: a case report
Sarah Quais, Ammar Suhail
Published: March 27, 2023 Explor Musculoskeletal Dis. 2023;1:31–36
Open Access
Editorial
Quality of care, referral, and early diagnosis of axial spondyloarthritis
Jürgen Braun ... Xenofon Baraliakos
Published: April 12, 2023 Explor Musculoskeletal Dis. 2023;1:37–42
Open Access
Review
Is there a place for magnetic resonance imaging in diffuse idiopathic skeletal hyperostosis?
Iris Eshed
Published: April 27, 2023 Explor Musculoskeletal Dis. 2023;1:43–53
This article belongs to the special issue Diffuse Idiopathic Skeletal Hyperostosis- A common but neglected disease
Open Access
Original Article
Quantitative magnetic resonance spectroscopy and imaging analysis of the lipid content in the psoas major and its association with intervertebral disc degeneration: a cross-sectional study
Izaya Ogon ... Atsushi Teramoto
Published: June 29, 2023 Explor Musculoskeletal Dis. 2023;1:54–63

Open Access
Letter to the Editor
Patient self-sampling for remote human leucocyte antigen-B27 analysis
Hannah Labinsky ... Johannes Knitza
Published: June 30, 2023 Explor Musculoskeletal Dis. 2023;1:64–67
This article belongs to the special issue Digital health technologies in rheumatology: emerging evidence and innovation

Open Access
Original Article
Morphological variations at the knee associated with osteoarthritis: a case-control study using data from the GOAL study
Anand Ramachandran Nair ... Abhishek Abhishek
Published: June 30, 2023 Explor Musculoskeletal Dis. 2023;1:68–76
Open Access
Editorial
Opening editorial for exploration in musculoskeletal diseases
Fernando Perez-Ruiz
Published: January 01, 2023 Explor Musculoskeletal Dis. 2023;1:1–3

Open Access
Review
Interstitial lung disease in patients with rheumatoid arthritis: a narrative review
Gloria Candelas Rodríguez, Virginia Villaverde
Published: October 20, 2023 Explor Musculoskeletal Dis. 2023;1:128–142
This article belongs to the special issue Comorbidities in rheumatoid arthritis
Open Access
Review
Genetic basis for skeletal new bone formation
Bruna Parreira ... Jácome Bruges-Armas
Published: October 23, 2023 Explor Musculoskeletal Dis. 2023;1:143–170
This article belongs to the special issue Diffuse Idiopathic Skeletal Hyperostosis- A common but neglected disease
Open Access
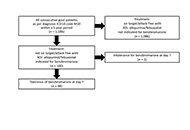
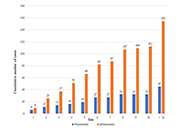
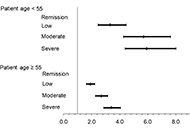
Original Article
Lessons to be learned from real life data based on 98 gout patients using benzbromarone
Ioana Hotea ... Tim L. Jansen
Published: October 30, 2023 Explor Musculoskeletal Dis. 2023;1:171–179
Open Access
Perspective
Nutritional problems in rheumatoid arthritis patients with temporomandibular joint involvement
Manolya Ilhanli, Ilker Ilhanli
Published: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:180–185
This article belongs to the special issue Comorbidities in rheumatoid arthritis
Open Access
Original Article
Association of mutations in hemochromatosis genes with clinical severity of calcium pyrophosphate arthritis
Joana Atxotegi-Saenz de Buruaga ... Fernando Perez-Ruiz
Published: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:186–193
Open Access
Review
Diffuse idiopathic skeletal hyperostosis and axial spondyloarthritis—similarities and differences
David Kiefer ... Xenofon Baraliakos
Published: November 20, 2023 Explor Musculoskeletal Dis. 2023;1:194–206
This article belongs to the special issue Diffuse Idiopathic Skeletal Hyperostosis- A common but neglected disease

Open Access
Original Article
Relationship between tendon elastography and clinical and ultrasound enthesitis scores in patients with psoriasis or psoriatic arthritis
Carlos A. Guillén-Astete ... Mónica Vázquez-Díaz
Published: November 20, 2023 Explor Musculoskeletal Dis. 2023;1:207–215
Open Access
Review
Diffuse idiopathic skeletal hyperostosis, beyond the musculoskeletal system
Fabiola Atzeni ... Reuven Mader
Published: December 04, 2023 Explor Musculoskeletal Dis. 2023;1:216–227
This article belongs to the special issue Diffuse Idiopathic Skeletal Hyperostosis- A common but neglected disease
Open Access
Original Article
Impact of disease activity on patient-reported subjective cognitive decline in patients with rheumatoid arthritis
Ozlem Pala ... Joel M. Kremer
Published: December 05, 2023 Explor Musculoskeletal Dis. 2023;1:228–240
This article belongs to the special issue Comorbidities in rheumatoid arthritis

