Affiliation:
1Internal Medicine, University of Arkansas for Medical Sciences, Northwest Regional Campus, Fayetteville, AR 72703, USA
Email: sahilsabh12@gmail.com
ORCID: https://orcid.org/0009-0008-4660-2169
Affiliation:
1Internal Medicine, University of Arkansas for Medical Sciences, Northwest Regional Campus, Fayetteville, AR 72703, USA
ORCID: https://orcid.org/0009-0005-0649-5205
Affiliation:
1Internal Medicine, University of Arkansas for Medical Sciences, Northwest Regional Campus, Fayetteville, AR 72703, USA
ORCID: https://orcid.org/0009-0007-1690-8290
Affiliation:
2Neurology, Mercy Hospital Northwest Arkansas, Rogers, AR 72758, USA
ORCID: https://orcid.org/0009-0001-7351-8287
Affiliation:
3Internal Medicine, Mercy Hospital Northwest Arkansas, Rogers, AR 72758, USA
ORCID: https://orcid.org/0009-0008-7990-2539
Affiliation:
1Internal Medicine, University of Arkansas for Medical Sciences, Northwest Regional Campus, Fayetteville, AR 72703, USA
ORCID: https://orcid.org/0009-0007-1079-6232
Explor Cardiol. 2025;3:101261 DOl: https://doi.org/10.37349/ec.2025.101261
Received: April 09, 2025 Accepted: June 05, 2025 Published: June 11, 2025
Academic Editor: Hemachandra Reddy, Texas Tech University, United States
Cardiac papillary fibroelastoma (CPF) is a rare, benign cardiac tumor with a significant risk for embolic complications, most notably ischemic stroke. This paper presents a case of a 54-year-old woman with cryptogenic stroke ultimately attributed to a CPF on the aortic valve, discovered via transesophageal echocardiography (TEE) after an initial unremarkable transthoracic study. Following diagnosis, the patient was treated with anticoagulation and scheduled for surgical excision. Although often asymptomatic, CPF can present with life-threatening embolic events, underscoring the importance of timely diagnosis through high-resolution imaging, particularly TEE. Surgical excision remains the definitive treatment in symptomatic or high-risk cases, but management of incidental, asymptomatic tumors remains controversial due to the absence of formal guidelines. This paper emphasizes the need for heightened clinical suspicion of CPF in cryptogenic stroke and advocates for individualized treatment approaches based on tumor characteristics and embolic risk.
Cardiac papillary fibroelastoma (CPF) is a rare, benign primary cardiac tumor. Among cardiac neoplasms, it is second only to myxoma in terms of prevalence [1]. While often discovered incidentally as an asymptomatic entity, CPF has increased in significance in cardiovascular medicine due to its potential to cause embolic events, particularly strokes. This case report and systemic review examines existing literature on CPF, focusing on its epidemiology, pathophysiology, clinical manifestations, diagnostic approaches, evidence linking it to stroke, and management strategies, drawing from case reports, retrospective studies, and systematic reviews.
A 54-year-old female with no past medical history presents with abrupt, new-onset right face and arm numbness, right facial droop, and dysarthria. The patient says she has never experienced these symptoms before and developed the symptoms while speaking on the phone. On examination in the emergency department, the patient reported that the symptoms had resolved other than some right upper extremity numbness. NIHSS stroke scale on presentation to the ED was 1 point. The patient’s labs and vitals were within normal limits. EKG and cardiac telemetry showed sinus rhythm on admission and throughout hospital stay. Hemoglobin A1c (HbA1c) was 5.9 g/dL on admission. Lipid panel showed a low density lipoprotein (LDL) of 92 mg/dL. Magnetic resonance imaging (MRI) of the brain without contrast showed scattered, acute ischemic infarcts in the left middle cerebral artery distribution (Figure 1). Neurology was consulted, and the patient was started on aspirin 81 mg daily and clopidogrel 75 mg daily, in addition to atorvastatin 80 mg daily. Neurology recommended an echocardiography for further workup, which was unremarkable. However, cardiology was subsequently consulted and the patient underwent a transesophageal echocardiography (TEE), which showed a papillary fibroelastoma on the aortic valve (Figure 2), which is believed to be the cardiac source of embolus. The patient was subsequently started on apixaban 5 mg twice-a-day. In addition, cardiovascular surgery was consulted, and the patient is set to undergo mass excision with possible aortic valve repair in one month, after a planned cardiac catheterization. The patient was also referred for further hypercoagulability workup with hematology outpatient. NIHSS stroke scale on discharge remained 1 point.
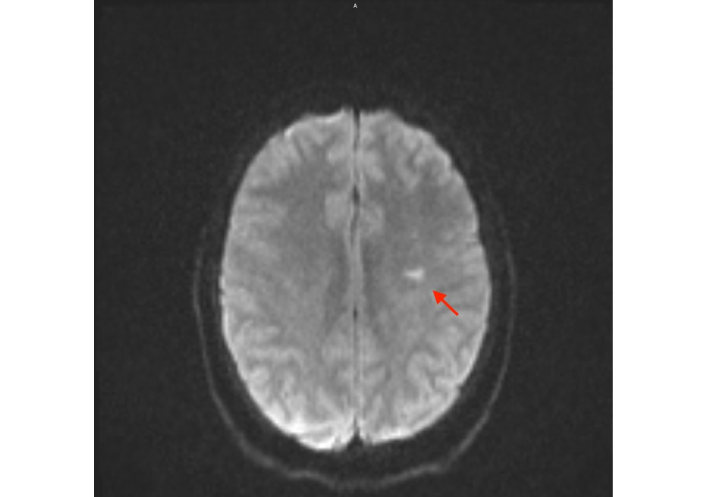
MRI of the brain without contrast showing multiple scattered, acute ischemic infarcts in the left middle cerebral artery distribution, the most prominent represented by the red arrow. MRI: magnetic resonance imaging
The association between CPF and stroke is well-documented, particularly in cryptogenic stroke cases where traditional risk factors are absent. It is estimated that 30–40% of CPF patients experience embolic events, a figure supported by retrospective analyses [2]. A key differential in cryptogenic stroke is CPF, noting that age is the only significant predictor of recurrent cerebrovascular events, with increasing age linked to higher log-odds of recurrence [3]. Further case studies provide compelling evidence, such as Helliwell et al. [4] (2020) who reported a patient with ischemic stroke treated with thrombolysis, followed by surgical excision of a CPF, with no recurrence post-intervention. The embolic mechanism is further solidified by histologic confirmation of tumor or thrombus emboli in cerebral vasculature, as seen by Liebeskind et al. [5] 2001 and Zurrú et al. [6] 2008.
Due to its asymptomatic nature, it is difficult to truly determine the prevalence of CPF. Based on autopsy and echocardiographic studies, the incidence is estimated to range from 0.001% to 0.33% [2]. Approximately 10% of all cardiac tumors are CPF [7]. Based on a systemic review analyzing 161 cases from 133 case reports and 11 case series, the mean age at diagnosis was identified to be 54.8 years with a slight male predominance (46.6%) [3]. In a large clinical study of acute ischemic cardioembolic stroke, ischemic stroke due to a cardiac tumor was only observed in 4 of 402 cases [8].
Historically, CPF has been characterized as an avascular, pedunculated tumor composed of collagen, elastic fibers, and smooth muscle cells, encased in a single endothelial layer [9]. It traditionally arises from the endocardium, with up to 80% of cases involving the aortic and mitral valves [10]. More specifically, 98.7% of CPFs were left-sided, with the mitral valve most commonly affected (38.9%), particularly the anterior leaflet (61.3%) [3]. As 91.4% of cases were independently mobile, its structure predisposes it to embolization through direct fragmentation or thrombus formation secondary to turbulent flow [2]. Given the tumor’s left-sided dominance, it is associated with systemic emboli, particularly to the cerebral circulation, rather than pulmonary emboli, which are rare due to the scarcity of right-sided CPFs.
Most tumors are incidental findings during imaging or autopsy. However, symptomatic cases may arise with embolic complications, which can be life-threatening. Among symptomatic patients, 32.3% experienced transient ischemic attacks (TIAs), while 67.8% presented with stroke, with multiple brain sites being the most common territory affected (36.6%) [3]. Other case reports have further illustrated this association, including Liebeskind et al. [5] (2001) who described a patient with cardioembolic stroke attributed to CPF, confirmed by histologic evidence of tumor emboli. Zurrú et al. [6] (2008) also documented a similar case with embolic stroke as the initial presentation. CPF may less commonly cause angina, sudden cardiac death from coronary ostial occlusion, or heart failure from valvular obstruction. However, these are often overshadowed by its cerebrovascular impact [10].
The gold standard in diagnostics for CPF diagnosis is echocardiography. Although transthoracic echocardiography (TTE) offers a sensitivity of 60–90%, TEE offers a near-100% sensitivity, particularly for smaller tumors (< 1 cm) or those in the left atrium, and thus remains the true gold standard [2]. This difference in sensitivity is further highlighted by a study that noted that 10.6% of CPFs were missed by TTE but detected by TEE, emphasizing TEE’s superior resolution [3]. On imaging, CPF can be distinguished from thrombi, myxomas or vegetations as it appears as a small (mean size 11.8 mm), mobile, pedunculated mass with a “frond-like” or “sea anemone” appearance [10]. Cardiac MRI and CT can be used as adjunctive tools, though are usually not needed or indicated due to echocardiography’s efficacy. If clinical doubt remains despite appropriate workup, accurate diagnosis may require clinical correlation and, in some cases, surgical pathology.
Given there are no formal guidelines from the American Heart Association (AHA) or European Society of Cardiology (ESC), management of CPF varies based on symptomatology and tumor characteristics. The primary approach for left-sided CPFs causing stroke or TIA is surgical excision, with 66.7% undergoing simple excision, 16.7% requiring valve repair, and 16.7% needing valve replacement. Medical approaches pre- and post-surgery varies as antiplatelet therapy was used in 87.9% of cases, while anticoagulation was employed in 12.1% [3]. Management of surrounding asymptomatic cases of CPFs remains controversial. Klarich et al. [2], 1997 suggested conservative management with anticoagulation or antiplatelet therapy for small, non-mobile tumors, but Helliwell et al. [4] (2020) and others argue for surgical resection of mobile or large (> 1 cm) left-sided CPFs due to their embolic potential, even in asymptomatic cases. The need for individualized decision-making on a case-by-case basis, understanding surgical risks versus embolic risks, is further underscored by the lack of randomized trials and standardized, consensus-based guidelines.
CPF is a benign tumor with a notable capacity to cause strokes through embolization, supported by a growing body of literature. The gold standard for diagnosis is echocardiography, particularly TEE. While the standard, definitive treatment for symptomatic cases is surgical excision, the management of asymptomatic patients remains controversial, as there is no standardized approach. The literature on CPF and its association with stroke is limited by small retrospective studies and reliance on case reports to guide management. Further studies, including larger, prospective studies, are needed to further elucidate embolic risk and define therapeutic strategies, especially in asymptomatic patients, to ensure ideal outcomes for this rare but impactful condition.
CPF: cardiac papillary fibroelastoma
MRI: magnetic resonance imaging
TEE: transesophageal echocardiography
SS: Conceptualization, Investigation, Writing—original draft, Writing—review & editing, Data curation. DHB and EHB: Investigation. PK, TT, and SA: Supervision, Validation, Writing—review & editing. All authors read and approved the submitted version.
The authors declare that they have no conflicts of interest.
This study adheres to the Declaration of Helsinki. According to the UAMS IRB, case reports are not classified as Human Subject Research and therefore do not require IRB review or approval.
Informed consent to participate in the study was obtained from all participants.
Informed consent to publication was obtained from relevant participants.
The data of this manuscript could be available from the corresponding authors upon reasonable request.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1727
Download: 150
Times Cited: 0
