Calcium pyrophosphate deposition disease: points to be considered for quality assurance in clinical practice
Calcium pyrophosphate deposition disease is known as crowned dens syndrome or peripheral arthritis, especially of knees, hips and shoulders. The disease course is asymptomatic, with acute or chronic
[...] Read more.
Calcium pyrophosphate deposition disease is known as crowned dens syndrome or peripheral arthritis, especially of knees, hips and shoulders. The disease course is asymptomatic, with acute or chronic disease activity related to osteoarthritis, especially in the elderly. Other risk factors are joint injury, osteoarthritis and metabolic conditions such as primary hyperparathyroidism, hemochromatosis, hypophosphatasia and hypomagnesemia. Genetic background should be considered before the age of 55 years. Only recently was the value of signs and symptoms weighted, allowing the introduction of classification criteria. Biomarkers include compensated polarized light microscopy findings, laboratory values and imaging. Imaging evidence refers to calcification of the fibrocartilage or hyaline cartilage. Chondrocalcinosis defined as such cartilage calcification is most commonly due to calcium pyrophosphate deposition disease. Calcification of the synovial membrane, joint capsule, or tendon should not be scored. Ultrasonography detects calcium pyrophosphate deposits with more than 80% sensitivity rates, which is superior to conventional radiography. In the future, dual-energy computerized tomography and Raman spectroscopy are promising new techniques to assess disease activity. Currently, the primary therapeutic goal is controlling inflammatory reactions and preventing further episodes. However, only hydroxychloroquine and magnesium carbonate have shown some efficacy and reduction of pain intensity so far. As patients report more significant unmet treatment needs than patients with gout, education is an essential issue of care. The new classification criteria will allow the validation of standardized outcome parameters with the definition of remission and low disease activity for developing treat-to-target strategies to perform well-designed interventional trials evaluating new treatment options and strategies.
Michael Schirmer, Johannes Dominikus Pallua
View:558
Download:12
Times Cited: 0
Calcium pyrophosphate deposition disease is known as crowned dens syndrome or peripheral arthritis, especially of knees, hips and shoulders. The disease course is asymptomatic, with acute or chronic disease activity related to osteoarthritis, especially in the elderly. Other risk factors are joint injury, osteoarthritis and metabolic conditions such as primary hyperparathyroidism, hemochromatosis, hypophosphatasia and hypomagnesemia. Genetic background should be considered before the age of 55 years. Only recently was the value of signs and symptoms weighted, allowing the introduction of classification criteria. Biomarkers include compensated polarized light microscopy findings, laboratory values and imaging. Imaging evidence refers to calcification of the fibrocartilage or hyaline cartilage. Chondrocalcinosis defined as such cartilage calcification is most commonly due to calcium pyrophosphate deposition disease. Calcification of the synovial membrane, joint capsule, or tendon should not be scored. Ultrasonography detects calcium pyrophosphate deposits with more than 80% sensitivity rates, which is superior to conventional radiography. In the future, dual-energy computerized tomography and Raman spectroscopy are promising new techniques to assess disease activity. Currently, the primary therapeutic goal is controlling inflammatory reactions and preventing further episodes. However, only hydroxychloroquine and magnesium carbonate have shown some efficacy and reduction of pain intensity so far. As patients report more significant unmet treatment needs than patients with gout, education is an essential issue of care. The new classification criteria will allow the validation of standardized outcome parameters with the definition of remission and low disease activity for developing treat-to-target strategies to perform well-designed interventional trials evaluating new treatment options and strategies.
 Work-related musculoskeletal disorders among surgeons: a bibliometric analysis from 1982 to 2024Open AccessReviewSurgeons are exposed to a high prevalence of work-related musculoskeletal disorders (WMSDs). The scientific issues surrounding this problem are generating a growing body of work. The aim of this stu [...] Read more.Philippe Gorce, Julien Jacquier-BretPublished: July 30, 2024 Explor Musculoskeletal Dis. 2024;2:317–335
Work-related musculoskeletal disorders among surgeons: a bibliometric analysis from 1982 to 2024Open AccessReviewSurgeons are exposed to a high prevalence of work-related musculoskeletal disorders (WMSDs). The scientific issues surrounding this problem are generating a growing body of work. The aim of this stu [...] Read more.Philippe Gorce, Julien Jacquier-BretPublished: July 30, 2024 Explor Musculoskeletal Dis. 2024;2:317–335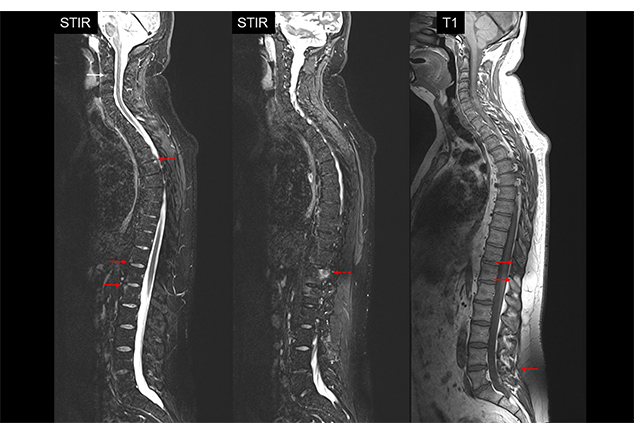 Axial spondyloarthritis—current aspectsOpen AccessReviewAxial spondyloarthritis (axSpA) is a frequent inflammatory rheumatic disease mainly affecting the axial skeleton causing inflammatory back pain. If chronic inflammation persists new bone formation may occur possibly leading to irr [...] Read more.Jürgen Braun, Denis PoddubnyyPublished: July 24, 2024 Explor Musculoskeletal Dis. 2024;2:300–316
Axial spondyloarthritis—current aspectsOpen AccessReviewAxial spondyloarthritis (axSpA) is a frequent inflammatory rheumatic disease mainly affecting the axial skeleton causing inflammatory back pain. If chronic inflammation persists new bone formation may occur possibly leading to irr [...] Read more.Jürgen Braun, Denis PoddubnyyPublished: July 24, 2024 Explor Musculoskeletal Dis. 2024;2:300–316 Sarcopenia, a hidden comorbidity of established rheumatoid arthritisOpen AccessEditorialThis editorial, “Sarcopenia: a hidden comorbidity of established rheumatoid arthritis” emphasizes the critical role of addressing comorbidities in rheumatoid arthritis (RA) management, focusing particularly on the clinical imp [...] Read more.Joan M. NollaPublished: July 19, 2024 Explor Musculoskeletal Dis. 2024;2:293–299
Sarcopenia, a hidden comorbidity of established rheumatoid arthritisOpen AccessEditorialThis editorial, “Sarcopenia: a hidden comorbidity of established rheumatoid arthritis” emphasizes the critical role of addressing comorbidities in rheumatoid arthritis (RA) management, focusing particularly on the clinical imp [...] Read more.Joan M. NollaPublished: July 19, 2024 Explor Musculoskeletal Dis. 2024;2:293–299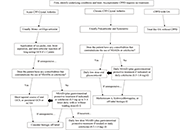 Treatment strategies for calcium pyrophosphate deposition diseaseOpen AccessReviewCalcium pyrophosphate deposition disease (CPPD) is a cause of inflammatory arthropathy that increases in prevalence with increasing age, presents in acute and chronic forms, and is characterized by [...] Read more.Anna J. Turlej, Angelo L. GaffoPublished: July 19, 2024 Explor Musculoskeletal Dis. 2024;2:279–292
Treatment strategies for calcium pyrophosphate deposition diseaseOpen AccessReviewCalcium pyrophosphate deposition disease (CPPD) is a cause of inflammatory arthropathy that increases in prevalence with increasing age, presents in acute and chronic forms, and is characterized by [...] Read more.Anna J. Turlej, Angelo L. GaffoPublished: July 19, 2024 Explor Musculoskeletal Dis. 2024;2:279–292 Calcium pyrophosphate deposition disease: points to be considered for quality assurance in clinical practiceOpen AccessReviewCalcium pyrophosphate deposition disease is known as crowned dens syndrome or peripheral arthritis, especially of knees, hips and shoulders. The disease course is asymptomatic, with acute or chronic [...] Read more.Michael Schirmer, Johannes Dominikus PalluaPublished: July 18, 2024 Explor Musculoskeletal Dis. 2024;2:270–278
Calcium pyrophosphate deposition disease: points to be considered for quality assurance in clinical practiceOpen AccessReviewCalcium pyrophosphate deposition disease is known as crowned dens syndrome or peripheral arthritis, especially of knees, hips and shoulders. The disease course is asymptomatic, with acute or chronic [...] Read more.Michael Schirmer, Johannes Dominikus PalluaPublished: July 18, 2024 Explor Musculoskeletal Dis. 2024;2:270–278 Screening for developmental dysplasia of the hip in Greece: current practice and future perspectivesOpen AccessMini ReviewScreening for developmental dysplasia of the hip (DDH) in Greece is being performed according to the guidelines issued by the Institute of Child Health in 2015. Screening strategies include universa [...] Read more.Konstantinos Chlapoutakis ... Maria RaissakiPublished: July 18, 2024 Explor Musculoskeletal Dis. 2024;2:264–269
Screening for developmental dysplasia of the hip in Greece: current practice and future perspectivesOpen AccessMini ReviewScreening for developmental dysplasia of the hip (DDH) in Greece is being performed according to the guidelines issued by the Institute of Child Health in 2015. Screening strategies include universa [...] Read more.Konstantinos Chlapoutakis ... Maria RaissakiPublished: July 18, 2024 Explor Musculoskeletal Dis. 2024;2:264–269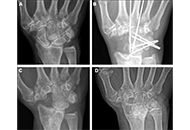 Progression of arthritis after four-corner fusion in patients with calcium pyrophosphate deposition disease: a case series of eleven patientsOpen AccessOriginal ArticleAim: The purpose of this study is to evaluate outcomes and radiographic progression of wrist arthritis after four-corner fusion (4CF) in patients with evidence of calcium pyrophosphate deposition [...] Read more.John F. Hoy ... Xavier C. SimcockPublished: July 10, 2024 Explor Musculoskeletal Dis. 2024;2:256–263
Progression of arthritis after four-corner fusion in patients with calcium pyrophosphate deposition disease: a case series of eleven patientsOpen AccessOriginal ArticleAim: The purpose of this study is to evaluate outcomes and radiographic progression of wrist arthritis after four-corner fusion (4CF) in patients with evidence of calcium pyrophosphate deposition [...] Read more.John F. Hoy ... Xavier C. SimcockPublished: July 10, 2024 Explor Musculoskeletal Dis. 2024;2:256–263