Interstitial lung disease in patients with rheumatoid arthritis: a narrative review
Rheumatoid arthritis (RA) is a chronic immune-mediated inflammatory disease of unknown origin. Although it mainly affects joints, it can have extra-articular manifestations, with the lung being one
[...] Read more.
Rheumatoid arthritis (RA) is a chronic immune-mediated inflammatory disease of unknown origin. Although it mainly affects joints, it can have extra-articular manifestations, with the lung being one of the most affected organs. The estimated incidence of diffuse interstitial lung disease (ILD) is 4 cases to 4.5 cases/1000 patient-years. The most common forms are usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP; 44–46% and 33–44%, respectively), although there have been reports of cases involving all the histopathologic forms described for the disease. RA-ILD is associated with specific risk factors, such as male sex, older age, smoking, and positive rheumatoid factor (RF) and anti-citrullinated peptide antibody (ACPA) levels. The clinical course of ILD ranges from asymptomatic forms to rapidly progressive disease in a minority of cases. It has been estimated that the risk of death is up to 3-fold higher in patients with RA-ILD than in those without ILD, making RA-ILD the second most common cause of death after cardiovascular disease. Treatment of RA has improved considerably in recent years with the advent of biologics; however, the use of these agents has been restricted in patients with ILD owing to safety concerns. Many doubts continue to surround the treatment of patients with RA-ILD. Therefore, the objective of this review is to examine the current management of affected patients in terms of diagnosis, treatment, and follow-up.
Gloria Candelas Rodríguez, Virginia Villaverde
View:2743
Download:81
Times Cited: 0
Rheumatoid arthritis (RA) is a chronic immune-mediated inflammatory disease of unknown origin. Although it mainly affects joints, it can have extra-articular manifestations, with the lung being one of the most affected organs. The estimated incidence of diffuse interstitial lung disease (ILD) is 4 cases to 4.5 cases/1000 patient-years. The most common forms are usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP; 44–46% and 33–44%, respectively), although there have been reports of cases involving all the histopathologic forms described for the disease. RA-ILD is associated with specific risk factors, such as male sex, older age, smoking, and positive rheumatoid factor (RF) and anti-citrullinated peptide antibody (ACPA) levels. The clinical course of ILD ranges from asymptomatic forms to rapidly progressive disease in a minority of cases. It has been estimated that the risk of death is up to 3-fold higher in patients with RA-ILD than in those without ILD, making RA-ILD the second most common cause of death after cardiovascular disease. Treatment of RA has improved considerably in recent years with the advent of biologics; however, the use of these agents has been restricted in patients with ILD owing to safety concerns. Many doubts continue to surround the treatment of patients with RA-ILD. Therefore, the objective of this review is to examine the current management of affected patients in terms of diagnosis, treatment, and follow-up.
 Association of mutations in hemochromatosis genes with clinical severity of calcium pyrophosphate arthritisOpen AccessOriginal ArticleAims: To study factors associated with the development of calcium pyrophosphate (CPP) arthritis and the severity phenotype. Methods: Transversal case-control study. Cases had to be confirme [...] Read more.Joana Atxotegi-Saenz de Buruaga ... Fernando Perez-RuizPublished: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:186–193
Association of mutations in hemochromatosis genes with clinical severity of calcium pyrophosphate arthritisOpen AccessOriginal ArticleAims: To study factors associated with the development of calcium pyrophosphate (CPP) arthritis and the severity phenotype. Methods: Transversal case-control study. Cases had to be confirme [...] Read more.Joana Atxotegi-Saenz de Buruaga ... Fernando Perez-RuizPublished: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:186–193 Nutritional problems in rheumatoid arthritis patients with temporomandibular joint involvementOpen AccessPerspectiveRheumatoid arthritis (RA) is an inflammatory arthritis that affects synovial joints, and it is not surprising that the temporomandibular joint (TMJ), a synovial joint, is also affected. However, TMJ [...] Read more.Manolya Ilhanli, Ilker IlhanliPublished: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:180–185
Nutritional problems in rheumatoid arthritis patients with temporomandibular joint involvementOpen AccessPerspectiveRheumatoid arthritis (RA) is an inflammatory arthritis that affects synovial joints, and it is not surprising that the temporomandibular joint (TMJ), a synovial joint, is also affected. However, TMJ [...] Read more.Manolya Ilhanli, Ilker IlhanliPublished: October 31, 2023 Explor Musculoskeletal Dis. 2023;1:180–185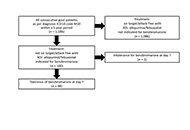 Lessons to be learned from real life data based on 98 gout patients using benzbromaroneOpen AccessOriginal ArticleAim: This study aims to analyze the efficacy and safety of benzbromarone as uricosuric, in a real-life clinical setting of a retrospective hospital-based gout cohort. Methods: Data from gou [...] Read more.Ioana Hotea ... Tim L. JansenPublished: October 30, 2023 Explor Musculoskeletal Dis. 2023;1:171–179
Lessons to be learned from real life data based on 98 gout patients using benzbromaroneOpen AccessOriginal ArticleAim: This study aims to analyze the efficacy and safety of benzbromarone as uricosuric, in a real-life clinical setting of a retrospective hospital-based gout cohort. Methods: Data from gou [...] Read more.Ioana Hotea ... Tim L. JansenPublished: October 30, 2023 Explor Musculoskeletal Dis. 2023;1:171–179 Genetic basis for skeletal new bone formationOpen AccessReviewBone formation is a complex process that occurs throughout life, and is normally limited to the skeletal system. In bone formation, osteoprogenitor cells follow several developmental stages, includi [...] Read more.Bruna Parreira ... Jácome Bruges-ArmasPublished: October 23, 2023 Explor Musculoskeletal Dis. 2023;1:143–170
Genetic basis for skeletal new bone formationOpen AccessReviewBone formation is a complex process that occurs throughout life, and is normally limited to the skeletal system. In bone formation, osteoprogenitor cells follow several developmental stages, includi [...] Read more.Bruna Parreira ... Jácome Bruges-ArmasPublished: October 23, 2023 Explor Musculoskeletal Dis. 2023;1:143–170 Interstitial lung disease in patients with rheumatoid arthritis: a narrative reviewOpen AccessReviewRheumatoid arthritis (RA) is a chronic immune-mediated inflammatory disease of unknown origin. Although it mainly affects joints, it can have extra-articular manifestations, with the lung being one [...] Read more.Gloria Candelas Rodríguez, Virginia VillaverdePublished: October 20, 2023 Explor Musculoskeletal Dis. 2023;1:128–142
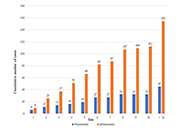
Interstitial lung disease in patients with rheumatoid arthritis: a narrative reviewOpen AccessReviewRheumatoid arthritis (RA) is a chronic immune-mediated inflammatory disease of unknown origin. Although it mainly affects joints, it can have extra-articular manifestations, with the lung being one [...] Read more.Gloria Candelas Rodríguez, Virginia VillaverdePublished: October 20, 2023 Explor Musculoskeletal Dis. 2023;1:128–142 Prevalence and factors associated to diffuse idiopathic skeletal hyperostosis in goutOpen AccessOriginal ArticleAim: To evaluate the prevalence, associated factors, and the impact of diffuse idiopathic skeletal hyperostosis (DISH) in patients with gout. Methods: Patients with gout entering into an in [...] Read more.Fernando Pérez-Ruiz ... Ana María Herrero-BeitesPublished: September 27, 2023 Explor Musculoskeletal Dis. 2023;1:121–127
Prevalence and factors associated to diffuse idiopathic skeletal hyperostosis in goutOpen AccessOriginal ArticleAim: To evaluate the prevalence, associated factors, and the impact of diffuse idiopathic skeletal hyperostosis (DISH) in patients with gout. Methods: Patients with gout entering into an in [...] Read more.Fernando Pérez-Ruiz ... Ana María Herrero-BeitesPublished: September 27, 2023 Explor Musculoskeletal Dis. 2023;1:121–127