Affiliation:
1Hepatobiliary Division, Department of Internal Medicine, Dr. Cipto Mangunkusumo National General Hospital, Faculty of Medicine, Universitas Indonesia, Jakarta 10430, Indonesia
2Digestive Disease and GI Oncology Center, Medistra Hospital, Jakarta 12950, Indonesia
Email: medicaldr2001id@yahoo.com
ORCID: https://orcid.org/0000-0001-9992-9968
Affiliation:
1Hepatobiliary Division, Department of Internal Medicine, Dr. Cipto Mangunkusumo National General Hospital, Faculty of Medicine, Universitas Indonesia, Jakarta 10430, Indonesia
ORCID: https://orcid.org/0000-0003-0614-0517
Affiliation:
3Department of Community Medicine, Faculty of Medicine, Universitas Indonesia, Jakarta 10430, Indonesia
ORCID: https://orcid.org/0000-0003-0413-2011
Affiliation:
1Hepatobiliary Division, Department of Internal Medicine, Dr. Cipto Mangunkusumo National General Hospital, Faculty of Medicine, Universitas Indonesia, Jakarta 10430, Indonesia
ORCID: https://orcid.org/0000-0001-8704-4716
Explor Dig Dis. 2025;4:100576 DOl: https://doi.org/10.37349/edd.2025.100576
Received: December 02, 2024 Accepted: April 22, 2025 Published: May 28, 2025
Academic Editor: Agustín Albillos, University of Alcalá, Spain
Background: Esophageal varices (EV) and gastric varices (GV) are the most common portal hypertension complications in liver cirrhosis patients. Esophagogastroduodenoscopy (EGD) is the main standard procedure for variceal screening and treatment. Nonetheless, luminal evaluation sometimes cannot accurately evaluate the size of varices. Recently, endoscopic ultrasound (EUS) has been studied for EV and GV evaluation.
Methods: Literature search was performed from PubMed, Scopus, and Cochrane Library databases until December 2022. Two independent reviewers (C.R.A.L. and T.P.) independently obtained and evaluated the selected studies according to pre-determined eligibility criteria.
Results: Ten studies (four observational studies, three randomized controlled trials, and three retrospective reviews of case series) describing 593 patients met our eligibility criteria. Eight out of ten studies evaluated utilization of EUS for coil embolization and/or cyanoacrylate injection. All studies demonstrated excellent technical success rate of the procedure with good therapeutic efficacy, in terms of lowering the risk of recurrent bleeding. Significantly better findings were observed from groups treated with combination of coil and cyanoacrylate glue injection in comparison to monotherapy. One study also highlighted the higher possibility of developing pulmonary embolism in groups treated with conventional cyanoacrylate injection.
Discussion: EUS-guided combination therapy appears to be a safe and effective modality for treating patients with gastric variceal bleeding with high number of complete obliteration and low risk of gastric variceal rebleeding. Further meta-analysis large-scale randomized clinical trials are still required to confirm these findings.
Esophageal varices (EV) and gastric varices (GV) are the most common portal hypertension complications in liver cirrhosis (LC) patient, where the presence of EV and GV are up to 50% and 20% in clinically significant portal hypertension (CSPH) condition [1]. Bleeding from gastroesophageal varices has been showed to have high mortality in LC patients [2–4]. Esophagogastroduodenoscopy (EGD) is the main standard procedure for variceal screening as well as variceal treatment. However, luminal evaluation sometimes cannot accurately evaluate the size of varices due to the possibility of deep EV, as well as GV identification for endoscopic treatment [5]. Recently, endoscopic ultrasound (EUS) has been studied for EV and GV evaluation [6]. Therefore, the authors would like to conduct a systematic review on the role of EUS in EV and GV management based on previous studies which have been done.
We search for the study from the PubMed, Scopus, and Cochrane Library databases until December 2022 with utilization of different search strings across those databases (Table 1, Figure 1). In order to improve the accuracy and focus of our search, as well as to ensure that no important studies were missed, we utilized Boolean operators and Medical Subject Headings (MeSH) keywords. The index terms for literature search included: “endoscopic ultrasound” AND “cyanoacrylate injection” AND “esophageal and gastric varices”. Secondary sources in the form of full-length articles were also examined from bibliographic review of the selected studies. Literature search was conducted and verified by two independent reviewers (C.R.A.L. and T.P.) by initial assessment of titles, abstracts, and full-text manuscript. No language restriction was applied in the search filter.
List of search strings utilized across various databases
| Databases | Search strings | Filters applied |
|---|---|---|
| PubMed | ((endoscopic ultrasound[Title/Abstract]) OR (EUS[Title/Abstract]) OR (endoscopic ultrasonography[Title/Abstract]) OR (endoscopic ultrasonographies[Title/Abstract]) OR (endosonography [Title/Abstract]) AND (cyanoacrylate[Title/Abstract])) OR (cyanoacrylate injection[Title/Abstract]) AND (esophageal varices[Title/Abstract]) AND (gastric varices[Title/Abstract]) | Publication date within 10 years |
| Scopus | (endoscopic ultrasound OR EUS OR endoscopic ultrasonography OR endoscopic ultrasonographies OR endosonography) AND (cyanoacrylate AND injection) AND (esophageal AND varices) AND (gastric AND varices) | Publication date within 10 years |
| Cochrane | ([MeSH descriptor: [Endosonography]] explode all trees) AND [([MeSH descriptor: [Cyanoacrylate]] explode all trees) AND ([MeSH descriptor: [Esophageal and Gastric Varices]] explode all trees) | Publication date within 10 years |
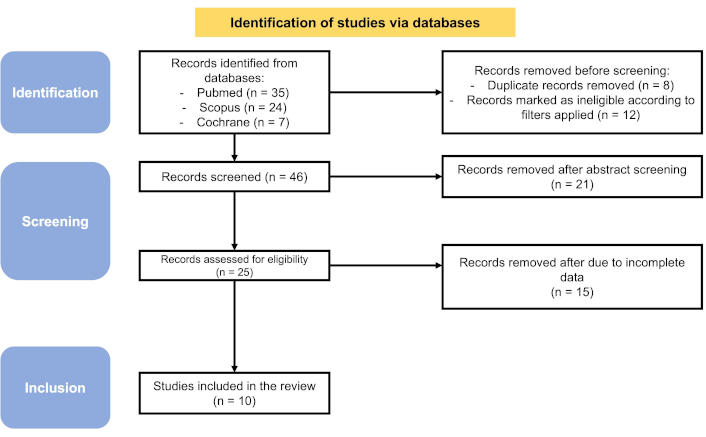
Data extraction process explained in PRISMA flow chart. Adapted from https://doi.org/10.1136/bmj.n71. CC BY
Two independent reviewers (C.R.A.L. and T.P.) independently obtained and evaluated the selected studies according to pre-determined eligibility criteria. Inclusion criteria were determined as follows: (1) a prospective or retrospective study designs or randomized controlled trials; adult participants (≥ 18 years old); (2) all patients with portal hypertension diagnosed based on imaging evaluation, EGD procedure, or hepatic vein pressure gradient (HVPG) measurement; (3) all patients who underwent EUS evaluation for the presence of EV or GV; (4) all patients who underwent EUS-guided vascular intervention therapy. Studies included in this review were published within the last one decade in order to extract data from the most recent evidence. Published studies were incorporated also from peer-reviewed articles and unpublished gray literatures. Exclusion criteria were any studies which evaluated procedures other than EUS. In addition, conference abstracts, abstracts from scientific posters, unpublished dissertations, unpublished theses, or presentation slides without any full-text manuscripts were also excluded considering the limited availability of complete data.
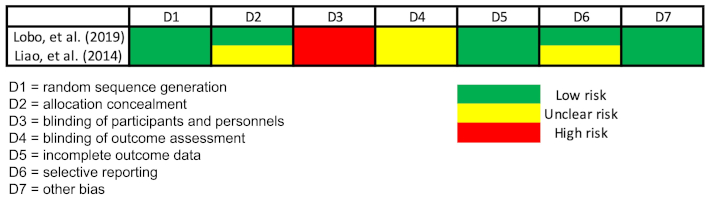
To ensure the methodological precision of our review, we also wrote our manuscript according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Assessment of study quality was done by evaluating the risk of bias in all studies. Quality assessment was conducted with Cochrane Risk of Bias Tool for randomized controlled trials (RoB-2) (Figure 2) [7, 8]. Since there is currently lack of validated tools available for evaluating the risk of bias in case series or uncontrolled cohort studies, we utilized the modified Newcastle Ottawa scale. Assessment of comparability and adjustment were excluded for uncontrolled studies. Qualitative assessment was then performed according to the list of questions in Table 2. Studies were assessed as good when no items gave a negative response; moderate when one item gave a negative response; and poor when at least two items gave negative responses. Any differences and/or disagreement between two independent reviewers were resolved by consensus-based discussion.
Assessment of risk of bias of the non-randomized studies
| Studies | Adequate case definition | Representativeness of the cases | Presence of all important data | Ascertainment of outcome | Risk of bias |
|---|---|---|---|---|---|
| Zheng, et al. (2019) [5] | Yes | No | Yes | Yes | Moderate |
| Robles-Medranda, et al. (2020) [9] | Yes | Yes | Yes | Yes | Low |
| Kouanda, et al. (2021) [10] | Yes | Yes | Yes | Yes | Low |
| Bazarbashi, et al. (2020) [11] | Yes | Yes | Yes | Yes | Low |
| Kozieł, et al. (2019) [12] | Yes | Yes | Yes | Yes | Low |
| Khoury, et al. (2018) [13] | Yes | Yes | Yes | No | Moderate |
| Bhat, et al. (2016) [14] | Yes | No | Yes | Yes | Moderate |
| Fujii-Lau, et al. (2015) [15] | Yes | Yes | Yes | No | Moderate |
The protocol for this systematic review will be registered with PROSPERO. PROSPERO ID is 1025880, registered on April 4th, 2025
After performing literature search and review of titles, abstracts, and contents, ten studies describing 593 patients met our eligibility criteria (Table 3). The included studies were published with the range of publication from year 2015 to 2020. The study designs included here were four observational studies, three randomized controlled trials, and three retrospective reviews of case series. Eight out of ten studies evaluated utilization of EUS for coil embolization and/or cyanoacrylate injection. One study utilized EUS for evaluating the presence of para-EV. In this study, two-channel therapeutic video-endoscope was used. Moreover, the author also assessed the effect of propranolol in the recurrence of varices within two years [8]. One study by Bazarbashi et al. [11] evaluated the combination of EUS-guided coil injection and hemostatic absorbable gelatin sponge [11]. Additionally, the follow-up period of each study ranged from 1 month until 1 year after enrollment of the subjects.
Summary of included studies
| No | Authors (year of publication) | Number of patients | Age (years) of the patients | Study design | Endoscopic treatment | Methods of examination | Study outcomes | Follow-up period |
|---|---|---|---|---|---|---|---|---|
| 1. | Zheng, et al. (2019) [5] | 153 | 55.2 ± 11.9 | Prospective cohort | Endoscopic variceal band ligation (EVL); endoscopic injection sclerotherapy (EIS); or EVL and EIS. | The endoscopy used for EUS probe examination was GIF-CV2o90, EU-ME1 ultrasound endoscopy host with UM-3R, 20-MHz catheter probe. | EVL group demonstrated significantly shorter time of recurrence compared to EIS and EIS + EVL groups (10 months vs 13 months vs 12 months, respectively). | Every 6 months for up to 3 years. |
| 2. | Robles-Medranda, et al. (2020) [9] | 60 | 61.8 ± 7.8 (coils + cyanoacrylate group) and 61.6 ± 12.3 (coils) | Single center, parallel-randomized controlled trial | EUS-guided coil embolization and cyanoacrylate injection vs EUS-guided coil embolization alone. | The EUS-guided procedure was conducted with a linear-array therapeutic echoendoscope (3.8 mm working channel) attached to an ultrasonography console. EUS-guided fine-needle puncture was performed with a 19-G needle. Coil deployment was performed (EUS-guided), followed by injection of 2-octyl-cyanoacrylate. Intravascular embolization was performed with Nester Embolization Coils (diameter: 10–16 mm. Straight length: 12–20 cm). | The technical success rate was outstanding (100%) in both treatments. Varices were immediately disappeared in 86.7% of the patients treated with coils and cyanoacrylate; while only 13.3% of the patients treated with coil alone experienced the outcome. Significantly higher number of re-bleeding events was observed in groups treated with coils alone (20%) compared to groups treated with coils and cyanoacrylate injection (3.3%). Significantly lower number of patients free from reintervention was observed in groups treated with coils alone compared to combined treatment (60% vs 83.3%, p = 0.01). | Three months after the initial procedure until up to 12 months after enrollment. |
| 3. | Lôbo, et al. (2019) [7] | 32 | 49.1 ± 14.83 in group treated with EUS-guided coil plus cyanoacrylate and 57.69 ± 11.56 in group treated with conventional cyanoacrylate | Randomized controlled trial | EUS-guided coil combined with cyanoacrylate injection. | Initially, conventional endoscopic examination was conducted to confirm the types of gastric varices and to assess the esophageal varices. EUS was then conducted with linear echoendoscope. Assessment of flow within the varices after each procedure was done by EUS with Doppler flow evaluation. | No significant difference was found in the events of varix thrombosis between both groups. Meanwhile, asymptomatic pulmonary embolism was more common to be found in group treated with conventional cyanoacrylate compared to group treated with combined therapy (50% vs 25%). | Average follow-up duration: 9 months |
| 4. | Liao, et al. (2014) [8] | 66 | 56–57 | Prospective randomized control study | Utilization of EUS to evaluate the presence of para-esophageal varices. | A two-channel therapeutic video-endoscope was used to perform endoscopy and EUS. The structure of para-esophageal and esophageal varices was assessed with a 12 MHz, radial type catheter ultrasound probe. | A significantly lower cumulative probability of recurrence within two years was observed in propranolol group (28%) compared to control (68%). In propranolol group, para-esophageal varices were also significantly regressed within 3 months. | Follow-up endoscopy and EUS were conducted every 3 months. |
| 5. | Kouanda, et al. (2021) [10] | 80 | 60.5 ± 10.4 | Single-center observational study | EUS-guided coil and cyanoacrylate injection. | EUS-guided coil and cyanoacrylate injection were performed under general anesthesia. All patients were given prophylactic intravenous antibiotics before the procedure. If the patients had high-risk esophageal varices, a conventional band ligation would be performed after gastric varices were successfully obliterated. | The technical success rate achieved in all procedures was 100%. 96.7% of the patients had obliterated varices throughout the endoscopic follow-up. Around 71.7% required 2 treatment sessions, 3.4% needed 4 treatment sessions, and 1.7% needed 5 sessions for the varices to be completely obliterated. | Surveillance endoscopy was conducted after 1 month, 3 months, and every 6 months. |
| 6. | Bazarbashi, et al. (2020) [11] | 10 | Mean age: 64 years old | Retrospective review of prospectively collected patients’ data. | EUS-guided coil injection combined with hemostatic absorbable gelatin sponge. | Initially, upper endoscopy was performed before EUS to evaluate active bleeding. After the upper endoscope was exchanged to a linear echoendoscope and gastric varices nest had been identified, transesophageal needle puncture (19-G) was used to perform transesophageal needle puncture. Multiple cylindrical-shaped coils would then be injected into the gastric varices nest (EUS-guided and fluoroscopy-guided). | Technical success rate was 100% for EUS-guided coil embolization without any intraprocedural complications. No evidence of absorbable gelatin sponge extrusion or formation of ulcer was reported. | Mean clinical follow-up days: 196 days (SD 110 days). A follow-up endoscopy was performed in all patients after a mean of 80 days (SD 33 days). |
| 7. | Kozieł, et al. (2019) [12] | 16 | 29–75 | Single-center retrospective study | EUS-guided coil and cyanoacrylate injection. | Initial evaluation with standard endoscopy. followed by assessment of varices with EUS. Next, varicose veins puncture and implantation of coil were performed with 19-G needles and 0.035-inch embolic coils. | Therapeutic success rate was achieved in 75% of the patients after the first procedure. 92% of the patients who were treated with EUS-guided coils and cyanoacrylate injection achieved therapeutic success. | Endoscopic and endosonography assessments at 1, 3, and 6 months. Average follow-up period: 327 days. |
| 8. | Khoury, et al. (2018) [13] | 10 | 13–80 | Retrospective case series | EUS-guided coiling | EUS-guided angiotherapy procedure was performed with a linear-array echoendoscope. Varices were accessed with a 19-G needle. A 50–10 mm-long and 8–15 mm-diameter synthetic, stainless steel fiber coil was then deployed. Some patients were injected with synthetic cyanoacrylate surgical glue after coil insertion. | Twenty-percent of the cases achieved complete eradication of gastric varices; while 50% of the cases accomplished near complete eradication of gastric varices. Around 30% of the patients needed another 1–2 coiling sessions to achieve a better response. | Average follow-up time: 9.7 months. |
| 9. | Bhat, et al. (2016) [14] | 152 | 19–88 | Retrospective observational study | EUS-guided coil and cyanoacrylate treatment. | The process began with intraluminal water filling of the gastric fundus. After that, echoendoscope will be positioned with transesophageal-transcrural approach or transgastric approach. Intravascular puncture of gastric fundal varices will then be directed by EUS. Embolization coils (diameter: 10–20 mm) will then be delivered along with immediate injection of cyanoacrylate. | Technical success rate was achieved in > 99% of the patients. From follow-up EUS examinations, 93% of the patients showed complete obliteration of gastric fundal varices. Approximately 3% of the patients suffered from re-bleeding. | Average follow-up: 436 days. |
| 10. | Fujii-Lau, et al. (2015) [15] | 14 | 51–72 | Retrospective observational study | EUS-guided variceal therapy with coil injection. | EUS procedure was performed with a curvilinear echoendoscope, fluoroscopy-guided. Prophylactic intravenous and post-procedure oral antibiotics were administered. | Eight out of fourteen patients did not experience any re-bleeding episode. Significant decrease of re-bleeding events was also observed in three patients with choledochal varices. | Median follow-up: 12 months. |
All studies demonstrated excellent technical success rate of the procedure [9–12], along with good therapeutic efficacy, including lower possibility of recurrence or re-bleeding episodes. Significantly better findings were observed from groups treated with combination of combination of coil and cyanoacrylate glue injection in comparison to monotherapy [1, 5, 8, 9, 12, 14, 15]. One randomized controlled trial by Lôbo et al. [7], however, showed no meaningful difference between both groups. Nevertheless, this study also highlighted the higher possibility of developing pulmonary embolism in groups treated with conventional cyanoacrylate injection [7]. A study by Liao et al. [8] also demonstrated the role of propranolol as an adjunctive therapy to lower cumulative probably of recurrence, as well as higher chance of para-EV regression [8].
As a common complication of portal hypertension, gastroesophageal variceal bleeding needs a more organized evidence-based management. Endoscopic-based management for gastroesophageal variceal bleeding was first introduced by Soehendra et al. [16] in 1986 through the application of glue injection for GV. Afterwards, more advanced therapeutic options; such as endoscopic-guided band ligation or ethanol injection or endoscopic therapy with tissue adhesive (e.g., N-butylcyanoacrylate) kept emerging [17]. In 1988, Stiegmann et al. [17] proposed endoscopic variceal ligation (EVL) as a therapeutic modality for EV. However, further evidences revealed that, in comparison to sclerotherapy, the rate of variceal bleeding recurrence after EVL was slightly higher. This shortcoming may be attributed to the inability of EVL to influence blood flow through esophageal collateral veins and perforators veins [18]. Initial treatment with cyanoacrylate had been indicated as a way to reduce the risk of gastroesophageal varices rebleeding. A systematic review and pooled analysis by Hu et al. [19] lower risk of rebleeding after cyanoacrylate injection.
Several drawbacks, nonetheless, are still found from existing modalities. For instance, a standard endoscopic examination may only evaluate the presence of superficial varices. Also, endoscopic glue injection, which had been recommended as one of the most preferrable therapeutic modalities for gastric variceal bleeding, may result into adverse complications; such as systemic or pulmonary embolization. On the other hand, aside from showing higher risk of recurrent variceal bleeding, the use of EVL also did not show any significant improvement in reducing HVPG, even when was compared to non-selective beta-blockers (NSBB). No statistically significant difference was also observed in mortality rate of groups treated with EVL compared to groups treated with NSBB [20].
Throughout the years, EUS has been having a more expanded role in the therapeutic fields for gastroesophageal varices [20–22]. Particularly, EUS allows the operator have an access towards abdominal arterial and venous vascular system without performing more invasive procedures; such as surgical approaches. Utilization of EUS may contribute to evaluate peri-gastric and perforating vessels. Application of color Doppler can also distinguish GV better from thickening of gastric folds or solid malignancies. In the application of glue injection, EUS allows the operator to identify and, subsequently, deliver glue injection to the perforating vessels more adequately. Moreover, attachment of synthetic fibers to coil may decrease the possibility of embolization by restricting the glue to varices. Application of coil can also be facilitated with EUS; thus, also protecting the splenorenal shunt, anatomically [20, 23]. A retrospective case series of four patients with gastric variceal bleeding and trans-jugular intrahepatic portosystemic shunts (TIPS) contraindications demonstrated technical and clinical success rate of EUS-guided hydro-coils without any adverse events related to the technical problems [22].
The use of combined treatment for GV itself has been introduced since 2011. Most of the studies in this review have indicated the superiority of combination therapy with coil placement and cyanoacrylate glue injection, in comparison to monotherapy. In 2013, a small cohort by Romero-Castro et al. [23] first demonstrated high obliteration rate of GV. Moreover, a meta-analysis by McCarty et al. [24] also showed that EUS-guided combination treatment can be a recommended therapeutic strategy for GV. A more updated meta-analysis by Baig et al. [20] showed high technical success of EUS-guided combination treatment (98.66%) with pooled rate of re-bleeding around 5.09%. Study by Hu et al. [19] in 2020 also highlighted lower risk of rebleeding after initial treatment with cyanoacrylate combined with other treatments (lipiodol, polidocanol, sclerotherapy, percutaneous transhepatic variceal embolization, ethanolamine, or TIPS), compared with monotherapy of cyanoacrylate. When being combined with EUS-guided coils, the pooled risk of rebleeding was 0.07, which was significantly lower compared to the pooled risk of rebleeding after administration of cyanoacrylate alone (0.15) [19].
Limitation of this systematic review, which may also become a major drawback of current available studies about EUS application on the management of gastroesophageal varices, is the lack of randomized controlled trials performed to examine the therapeutic efficacy of EUS-guided approaches. Several studies included in here were conducted as a retrospective case series with small number of patients. Consequently, more randomized clinical trials with larger sample size are still necessary to confirm the current findings.
Aside from the types of study, heterogeneity between studies and risk of bias were also considered as our limitations. Heterogeneity between studies was noticed especially in the age of the subjects. Studies by Kozieł et al. (2019) [12], Khoury et al. (2018) [13], and Bhat et al. (2016) [14] had wider range of age compared to other studies. Criteria of technical success rate, as well as the number of coiling sessions performed in each study might also contribute to the variability of results. For instance, Khoury et al. [13] demonstrated that approximately 30% of the subjects needed more than one EUS-guided coiling sessions to achieve better eradication of varices. This study, nevertheless, was performed only in a single center and still highlighted the benefit of cyanoacrylate injection as adjunctive therapy for GV. From our quality assessment, there were low-to-moderate risk of bias, particularly related to the representativeness of the case, ascertainment of outcome, and blinding process. From two randomized controlled trials, only one study by Lôbo et al. [7] clearly stated that the subjects had been blinded from the allocation. In these studies, blinding of the personnel and outcome assessment might not be applicable due to the necessity of follow-up after the procedures as well as the ethical issues which might be arisen if blinding was applied. While promising findings were found from this systematic review, the presence of potential biases and methodological limitations require further studies to increase the validity of the outcomes.
EUS-guided combination therapy appears to be a safe and effective modality for treating patients with gastric variceal bleeding with high number of complete obliteration and low risk of gastric variceal rebleeding. Further meta-analysis large-scale randomized clinical trials are still required to tackle the weakness of this study. As the demand of less invasive procedures keeps increasing throughout the years, EUS-guided therapy remains as a promising option for targeting problems in abdominal vasculature.
CSPH: clinically significant portal hypertension
EGD: esophagogastroduodenoscopy
EUS: endoscopic ultrasound
EV: esophageal varices
EVL: endoscopic variceal ligation
GV: gastric varices
HVPG: hepatic vein pressure gradient
LC: liver cirrhosis
MeSH: medical subject headings
NSBB: non-selective beta-blockers
TIPS: trans-jugular intrahepatic portosystemic shunts
CRAL: Conceptualization, Methodology, Data curation, Formal analysis, Writing—original draft, Writing—review & editing, Validation. MSP: Data curation, Formal analysis, Writing—original draft. TP: Methodology, Data curation, Formal analysis, Writing—original draft. RAG: Writing—review & editing, Validation.
Cosmas Rinaldi Adithya Lesmana is the Editorial Board Member of Exploration of Digestive Diseases. However, he had no involvement in the decision-making or the review process of this manuscript by the journal. The other authors declare no conflicts of interest.
Not applicable.
Not applicable.
Not applicable.
All data analyzed in this systematic review were obtained from publicly available studies in the PubMed, Scopus, and Cochrane Library. The full list of included studies with references is provided within this manuscript.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 2169
Download: 38
Times Cited: 0
