-
308 results in Exploration of Targeted Anti-tumor TherapySort byMost Viewed
 Current strategies for the design of PROTAC linkers: a critical reviewOpen AccessReviewPROteolysis TArgeting Chimeras (PROTACs) are heterobifunctional molecules consisting of two ligands; an “anchor” to bind to an E3 ubiquitin ligase and a “warhead” [...] Read more.Robert I. Troup ... Matthias G. J. BaudPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:273–312
Current strategies for the design of PROTAC linkers: a critical reviewOpen AccessReviewPROteolysis TArgeting Chimeras (PROTACs) are heterobifunctional molecules consisting of two ligands; an “anchor” to bind to an E3 ubiquitin ligase and a “warhead” [...] Read more.Robert I. Troup ... Matthias G. J. BaudPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:273–312
DOI: https://doi.org/10.37349/etat.2020.00018
This article belongs to the special issue Proteolysis Targeting Chimera (PROTAC) The impact of tumour pH on cancer progression: strategies for clinical interventionOpen AccessReviewDysregulation of cellular pH is frequent in solid tumours and provides potential opportunities for therapeutic intervention. The acidic microenvironment within a tumour can promote migration, invasi [...] Read more.Carol Ward ... Simon P LangdonPublished: April 28, 2020 Explor Target Antitumor Ther. 2020;1:71–100
The impact of tumour pH on cancer progression: strategies for clinical interventionOpen AccessReviewDysregulation of cellular pH is frequent in solid tumours and provides potential opportunities for therapeutic intervention. The acidic microenvironment within a tumour can promote migration, invasi [...] Read more.Carol Ward ... Simon P LangdonPublished: April 28, 2020 Explor Target Antitumor Ther. 2020;1:71–100
DOI: https://doi.org/10.37349/etat.2020.00005 Inhibitors of the Fanconi anaemia pathway as potential antitumour agents for ovarian cancerOpen AccessReviewThe Fanconi anaemia (FA) pathway is an important mechanism for cellular DNA damage repair, which functions to remove toxic DNA interstrand crosslinks. This is particularly relevant in the context of [...] Read more.Sarah J Taylor ... Simon P LangdonPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:26–52
Inhibitors of the Fanconi anaemia pathway as potential antitumour agents for ovarian cancerOpen AccessReviewThe Fanconi anaemia (FA) pathway is an important mechanism for cellular DNA damage repair, which functions to remove toxic DNA interstrand crosslinks. This is particularly relevant in the context of [...] Read more.Sarah J Taylor ... Simon P LangdonPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:26–52
DOI: https://doi.org/10.37349/etat.2020.00003 Development of PROTACs to address clinical limitations associated with BTK-targeted kinase inhibitorsOpen AccessReviewChronic lymphocytic leukemia is a common form of leukemia and is dependent on growth-promoting signaling via the B-cell receptor. The Bruton tyrosine kinase (BTK) is an important mediator of B-cell [...] Read more.Rachael Arthur ... Graham PackhamPublished: June 29, 2020 Explor Target Antitumor Ther. 2020;1:131–152
Development of PROTACs to address clinical limitations associated with BTK-targeted kinase inhibitorsOpen AccessReviewChronic lymphocytic leukemia is a common form of leukemia and is dependent on growth-promoting signaling via the B-cell receptor. The Bruton tyrosine kinase (BTK) is an important mediator of B-cell [...] Read more.Rachael Arthur ... Graham PackhamPublished: June 29, 2020 Explor Target Antitumor Ther. 2020;1:131–152
DOI: https://doi.org/10.37349/etat.2020.00009
This article belongs to the special issue Proteolysis Targeting Chimera (PROTAC) Novel approaches for the rational design of PROTAC linkersOpen AccessReviewProteolysis targeting chimeras (PROTACs) represent a promising class of hetero-bivalent molecules that facilitate ubiquitination of a target protein by simultaneously binding and bringing together b [...] Read more.Almaz Zagidullin ... Emil BulatovPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:381–390
Novel approaches for the rational design of PROTAC linkersOpen AccessReviewProteolysis targeting chimeras (PROTACs) represent a promising class of hetero-bivalent molecules that facilitate ubiquitination of a target protein by simultaneously binding and bringing together b [...] Read more.Almaz Zagidullin ... Emil BulatovPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:381–390
DOI: https://doi.org/10.37349/etat.2020.00023
This article belongs to the special issue Proteolysis Targeting Chimera (PROTAC) Early-stage triple negative breast cancer: the therapeutic role of immunotherapy and the prognostic value of pathological complete responseOpen AccessReviewTriple negative breast cancer (TNBC) represents an aggressive disease associated with a high risk of recurrence after curative treatment and a poor prognosis in the metastatic setting. Chemotherapy [...] Read more.Pierluigi De Santis ... Palma FedelePublished: February 28, 2024 Explor Target Antitumor Ther. 2024;5:232–250
Early-stage triple negative breast cancer: the therapeutic role of immunotherapy and the prognostic value of pathological complete responseOpen AccessReviewTriple negative breast cancer (TNBC) represents an aggressive disease associated with a high risk of recurrence after curative treatment and a poor prognosis in the metastatic setting. Chemotherapy [...] Read more.Pierluigi De Santis ... Palma FedelePublished: February 28, 2024 Explor Target Antitumor Ther. 2024;5:232–250
DOI: https://doi.org/10.37349/etat.2024.00215
This article belongs to the special issue Innovative Strategies to Target Triple-negative Breast Cancer Antibody-drug conjugates: beyond current approvals and potential future strategiesOpen AccessReviewThe recent approvals for antibody-drug conjugates (ADCs) in multiple malignancies in recent years have fuelled the ongoing development of this class of drugs. These novel agents combine the benefits [...] Read more.Siddharth Menon ... Hui K. GanPublished: April 28, 2022 Explor Target Antitumor Ther. 2022;3:252–277
Antibody-drug conjugates: beyond current approvals and potential future strategiesOpen AccessReviewThe recent approvals for antibody-drug conjugates (ADCs) in multiple malignancies in recent years have fuelled the ongoing development of this class of drugs. These novel agents combine the benefits [...] Read more.Siddharth Menon ... Hui K. GanPublished: April 28, 2022 Explor Target Antitumor Ther. 2022;3:252–277
DOI: https://doi.org/10.37349/etat.2022.00082
This article belongs to the special issue Antibody-Drug Conjugates PROTACs are effective in addressing the platelet toxicity associated with BCL-XL inhibitorsOpen AccessReviewBCL-XL is an anti-apoptotic protein that plays an important role in tumorigenesis, metastasis, and intrinsic or therapy-induced cancer drug resistance. More recently, BCL-XL has also been identified [...] Read more.Peiyi Zhang ... Guangrong ZhengPublished: August 31, 2020 Explor Target Antitumor Ther. 2020;1:259–272
PROTACs are effective in addressing the platelet toxicity associated with BCL-XL inhibitorsOpen AccessReviewBCL-XL is an anti-apoptotic protein that plays an important role in tumorigenesis, metastasis, and intrinsic or therapy-induced cancer drug resistance. More recently, BCL-XL has also been identified [...] Read more.Peiyi Zhang ... Guangrong ZhengPublished: August 31, 2020 Explor Target Antitumor Ther. 2020;1:259–272
DOI: https://doi.org/10.37349/etat.2020.00017
This article belongs to the special issue Proteolysis Targeting Chimera (PROTAC) Targeted inhibition of mRNA translation initiation factors as a novel therapeutic strategy for mature B-cell neoplasmsOpen AccessReviewCancer development is frequently associated with dysregulation of mRNA translation to enhance both increased global protein synthesis and translation of specific mRNAs encoding oncoproteins. Thus, t [...] Read more.Joe Taylor ... Graham PackhamPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:3–25
Targeted inhibition of mRNA translation initiation factors as a novel therapeutic strategy for mature B-cell neoplasmsOpen AccessReviewCancer development is frequently associated with dysregulation of mRNA translation to enhance both increased global protein synthesis and translation of specific mRNAs encoding oncoproteins. Thus, t [...] Read more.Joe Taylor ... Graham PackhamPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:3–25
DOI: https://doi.org/10.37349/etat.2020.00002 Potential benefit of β-glucans as adjuvant therapy in immuno-oncology: a reviewOpen AccessReviewFungal compounds have long been used for centuries as food supplements. β-glucans have been identified as the most interesting molecules with beneficial effects in several chronic diseas [...] Read more.Valeria Cognigni ... Rossana BerardiPublished: April 30, 2021 Explor Target Antitumor Ther. 2021;2:122–138
Potential benefit of β-glucans as adjuvant therapy in immuno-oncology: a reviewOpen AccessReviewFungal compounds have long been used for centuries as food supplements. β-glucans have been identified as the most interesting molecules with beneficial effects in several chronic diseas [...] Read more.Valeria Cognigni ... Rossana BerardiPublished: April 30, 2021 Explor Target Antitumor Ther. 2021;2:122–138
DOI: https://doi.org/10.37349/etat.2021.00036
This article belongs to the special issue Immunotherapy in Cancer Patients An overview of the anti-cancer actions of Tanshinones, derived from Salvia miltiorrhiza (Danshen)Open AccessReviewTanshinone is a herbal medicinal compound described in Chinese medicine, extracted from the roots of Salvia miltiorrhiza (Danshen). This family of compounds, including Tanshinone IIA and Tanshinone [...] Read more.Irum Naz ... Kwang Seok AhnPublished: June 29, 2020 Explor Target Antitumor Ther. 2020;1:153–170
An overview of the anti-cancer actions of Tanshinones, derived from Salvia miltiorrhiza (Danshen)Open AccessReviewTanshinone is a herbal medicinal compound described in Chinese medicine, extracted from the roots of Salvia miltiorrhiza (Danshen). This family of compounds, including Tanshinone IIA and Tanshinone [...] Read more.Irum Naz ... Kwang Seok AhnPublished: June 29, 2020 Explor Target Antitumor Ther. 2020;1:153–170
DOI: https://doi.org/10.37349/etat.2020.00010
This article belongs to the special issue Targeting Transcription Factors for Cancer Therapy Targeting HER2 in breast cancer: new drugs and paradigms on the horizonOpen AccessReviewAbout 15–20% of all breast cancers (BCs) are defined human epidermal growth factor receptor 2 (HER2)-positive, based on the overexpression of HER2 protein and/or amplification [...] Read more.Paolo Tarantino ... Giuseppe CuriglianoPublished: April 30, 2021 Explor Target Antitumor Ther. 2021;2:139–155
Targeting HER2 in breast cancer: new drugs and paradigms on the horizonOpen AccessReviewAbout 15–20% of all breast cancers (BCs) are defined human epidermal growth factor receptor 2 (HER2)-positive, based on the overexpression of HER2 protein and/or amplification [...] Read more.Paolo Tarantino ... Giuseppe CuriglianoPublished: April 30, 2021 Explor Target Antitumor Ther. 2021;2:139–155
DOI: https://doi.org/10.37349/etat.2021.00037 The clinical advances of proteolysis targeting chimeras in oncologyOpen AccessReviewProteolysis targeting chimeras (PROTACs) are a class of small molecules designed to target proteins for degradation. Their novel and unique modes of action provide PROTACs with the potential for the [...] Read more.Hao Xie ... Jason B. FlemingPublished: December 31, 2021 Explor Target Antitumor Ther. 2021;2:511–521
The clinical advances of proteolysis targeting chimeras in oncologyOpen AccessReviewProteolysis targeting chimeras (PROTACs) are a class of small molecules designed to target proteins for degradation. Their novel and unique modes of action provide PROTACs with the potential for the [...] Read more.Hao Xie ... Jason B. FlemingPublished: December 31, 2021 Explor Target Antitumor Ther. 2021;2:511–521
DOI: https://doi.org/10.37349/etat.2021.00061
This article belongs to the special issue Proteolysis Targeting Chimera (PROTAC) Targeting transcription factors in cancer drug discoveryOpen AccessReviewCancer drug discovery is currently dominated by clinical trials or clinical research. Several potential drug candidates have been brought into the pipeline of drug discovery after showing very promi [...] Read more.Partha MitraPublished: December 28, 2020 Explor Target Antitumor Ther. 2020;1:401–412
Targeting transcription factors in cancer drug discoveryOpen AccessReviewCancer drug discovery is currently dominated by clinical trials or clinical research. Several potential drug candidates have been brought into the pipeline of drug discovery after showing very promi [...] Read more.Partha MitraPublished: December 28, 2020 Explor Target Antitumor Ther. 2020;1:401–412
DOI: https://doi.org/10.37349/etat.2020.00025
This article belongs to the special issue Targeting Transcription Factors for Cancer Therapy The promising potential of piperlongumine as an emerging therapeutics for cancerOpen AccessReviewIn spite of the immense advancement in the diagnostic and treatment modalities, cancer continues to be one of the leading causes of mortality across the globe, responsible for the death of around 10 [...] Read more.Dey Parama ... Ajaikumar B. KunnumakkaraPublished: August 30, 2021 Explor Target Antitumor Ther. 2021;2:323–354
The promising potential of piperlongumine as an emerging therapeutics for cancerOpen AccessReviewIn spite of the immense advancement in the diagnostic and treatment modalities, cancer continues to be one of the leading causes of mortality across the globe, responsible for the death of around 10 [...] Read more.Dey Parama ... Ajaikumar B. KunnumakkaraPublished: August 30, 2021 Explor Target Antitumor Ther. 2021;2:323–354
DOI: https://doi.org/10.37349/etat.2021.00049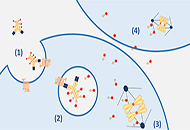 Advancing antibody-drug conjugates in gynecological malignancies: myth or reality?Open AccessReviewAntibody-drug conjugates (ADCs) represent a new class of therapeutic agents designed to target specific antigens on tumor cells, combining the specificity of monoclonal antibodies to the cytotoxicit [...] Read more.Marta Nerone ... Ilaria ColomboPublished: April 19, 2022 Explor Target Antitumor Ther. 2022;3:149–171
Advancing antibody-drug conjugates in gynecological malignancies: myth or reality?Open AccessReviewAntibody-drug conjugates (ADCs) represent a new class of therapeutic agents designed to target specific antigens on tumor cells, combining the specificity of monoclonal antibodies to the cytotoxicit [...] Read more.Marta Nerone ... Ilaria ColomboPublished: April 19, 2022 Explor Target Antitumor Ther. 2022;3:149–171
DOI: https://doi.org/10.37349/etat.2022.00077
This article belongs to the special issue Antibody-Drug Conjugates Colorectal cancer genomic biomarkers in the clinical management of patients with metastatic colorectal carcinomaOpen AccessReviewColorectal carcinoma (CRC) is an heterogeneous disease in which different genetic alterations play a role in its pathogenesis and progression and offer potential for therapeutic intervention. The re [...] Read more.Anna Maria Rachiglio ... Nicola NormannoPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:53–70
Colorectal cancer genomic biomarkers in the clinical management of patients with metastatic colorectal carcinomaOpen AccessReviewColorectal carcinoma (CRC) is an heterogeneous disease in which different genetic alterations play a role in its pathogenesis and progression and offer potential for therapeutic intervention. The re [...] Read more.Anna Maria Rachiglio ... Nicola NormannoPublished: February 29, 2020 Explor Target Antitumor Ther. 2020;1:53–70
DOI: https://doi.org/10.37349/etat.2020.00004 An overview of the potential anticancer properties of cardamoninOpen AccessReviewCancer is one of the leading causes of mortality, contributing to 9.6 million deaths globally in 2018 alone. Although several cancer treatments exist, they are often associated with severe side effe [...] Read more.Shanaya Ramchandani ... Manoj GargPublished: December 28, 2020 Explor Target Antitumor Ther. 2020;1:413–426
An overview of the potential anticancer properties of cardamoninOpen AccessReviewCancer is one of the leading causes of mortality, contributing to 9.6 million deaths globally in 2018 alone. Although several cancer treatments exist, they are often associated with severe side effe [...] Read more.Shanaya Ramchandani ... Manoj GargPublished: December 28, 2020 Explor Target Antitumor Ther. 2020;1:413–426
DOI: https://doi.org/10.37349/etat.2020.00026
This article belongs to the special issue Targeting Transcription Factors for Cancer Therapy Potential of guggulsterone, a farnesoid X receptor antagonist, in the prevention and treatment of cancerOpen AccessReviewCancer is one of the most dreadful diseases in the world with a mortality of 9.6 million annually. Despite the advances in diagnosis and treatment during the last couple of decades, it still remains [...] Read more.Sosmitha Girisa ... Ajaikumar B. KunnumakkaraPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:313–342
Potential of guggulsterone, a farnesoid X receptor antagonist, in the prevention and treatment of cancerOpen AccessReviewCancer is one of the most dreadful diseases in the world with a mortality of 9.6 million annually. Despite the advances in diagnosis and treatment during the last couple of decades, it still remains [...] Read more.Sosmitha Girisa ... Ajaikumar B. KunnumakkaraPublished: October 30, 2020 Explor Target Antitumor Ther. 2020;1:313–342
DOI: https://doi.org/10.37349/etat.2020.00019
This article belongs to the special issue Targeting Transcription Factors for Cancer Therapy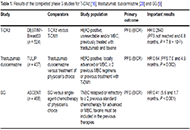 New antibody-drug conjugates (ADCs) in breast cancer—an overview of ADCs recently approved and in later stages of developmentOpen AccessReviewAntibody-drug conjugates (ADCs) have changed the treatment of breast cancer (BC) in more recent years. BC is a heterogenous group of malignancies with a broad range of histopathological characterist [...] Read more.Kira-Lee Koster ... Markus JoergerPublished: February 24, 2022 Explor Target Antitumor Ther. 2022;3:27–36
New antibody-drug conjugates (ADCs) in breast cancer—an overview of ADCs recently approved and in later stages of developmentOpen AccessReviewAntibody-drug conjugates (ADCs) have changed the treatment of breast cancer (BC) in more recent years. BC is a heterogenous group of malignancies with a broad range of histopathological characterist [...] Read more.Kira-Lee Koster ... Markus JoergerPublished: February 24, 2022 Explor Target Antitumor Ther. 2022;3:27–36
DOI: https://doi.org/10.37349/etat.2022.00069
This article belongs to the special issue Antibody-Drug Conjugates -
