Affiliation:
Department of Internal Medicine, Cardiology Division, Hypertension Section, University of Texas Southwestern Medical Center, Dallas, TX 75390, USA
Email: Shawna.Nesbitt@utsouthwestern.edu
ORCID: https://orcid.org/0000-0001-6043-6541
Explor Med. 2025;6:1001337 DOl: https://doi.org/10.37349/emed.2025.1001337
Received: February 16, 2025 Accepted: May 20, 2025 Published: June 23, 2025
Academic Editor: Carlos M. Ferrario, Wake Forest School of Medicine, USA
The article belongs to the special issue Drug Adherence in Hypertension
Major gaps in hypertension control continue despite effective treatments. Among patients who are diagnosed and treated, adherence to therapy remains a barrier to achieving and maintaining control. Multiple modalities have demonstrated success in facilitating adherence. Using fixed dose combination therapy and home self blood pressure (BP) monitoring are 2 major approaches offering significant advantages to improve adherence, lower BP, and ultimately improve outcomes. While no single modality is universal for all patients, exploring the advantages and challenges of these modalities is a key strategy to identify the ideal approach to achieve better BP control.
Blood pressure (BP) continues to be a major challenge in reducing cardiovascular (CV) events with persistent issues in diagnosis, awareness, and control. Many approaches have been proposed to improve BP control, yet the success is limited. Finding the best approach requires assessing the primary barrier in achieving control and aligning the problem with the proper solution.
Globally hypertension accounts for 10.8 million deaths and in 2019, it was the leading risk factor for the burden of disease, except in Oceana and some areas of sub-Saharan Africa [1]. Using the American Heart Association definition of hypertension [> 130/80 mmHg (> 17/10 kPa)], the overall prevalence of hypertension in the U.S. is 46%, while in adults over 65 years of age, it is 76.5%, 58.6% in 45–64 years of age, and 28.5% in 20–44 years of age. Hypertension is undiagnosed in 38% of adults and only 25% of U.S. hypertensives are under control [1].
Nonadherence contributes significantly to the lack of BP control with an overall nonadherence rate of 37% in patients with apparent treatment resistant hypertension. However, the method of data collection has a large effect on the reported rate. Whereas the prevalence of nonadherence was reported at 20% with indirect assessment using questionnaires and pill counts, when assessed by direct observation or therapeutic testing it was as high as 46% [2]. In a recent study assessing drug adherence by serum drug concentration in hypertensive Norwegian patients, poorer adherence was more common in younger patients, patients with higher pill burden and less combination therapy, and in individuals who were not of European descent [3].
The burden of uncontrolled hypertension is significant in human and financial costs [4]. Improving adherence to therapeutic recommendations can improve the lives of many and reduce CV outcomes. Multiple approaches to improve adherence to therapy have been studied with variable success rates. Here we explore 2 major approaches to improve adherence.
There is no doubt that simpler regimens yield better adherence. In this regard, combination therapy offers a true advantage to cost and pill burden for patients [5]. The evidence supporting the use of fixed dose combinations is strong. These options show higher persistence and significantly lower major CV events due to hypertension in large retrospective analyses. In a retrospective analysis of patients prescribed amlodipine/benazepril fixed dose combination compared to dihydropyridine calcium channel blocker (CCB)/angiotensin converting enzyme inhibitor as separate medications, the medication possession ratio was 88% versus 69% respectively (P < 0.001) [6]. Simonyi et al. [7] found that in a retrospective observational study of 173,206 patients with hypertension in the Hungarian health system, on each option of fixed dose ramipril/amlodipine combinations compared to free equivalent versions of treatment at 24 months, in addition to improved drug persistence (82–85% vs. 58–73%, respectively), the composite major adverse CV events were significantly reduced with fixed dose pills for each dose strength (hazard ratio 0.68–0.7, P < 0.001).
Most fixed dose combinations consist of 2 drug agents, however, fewer 3 drug combinations exist. Recently an international, randomized, double-blind, active-controlled, parallel-group 12-week trial comparing the triple combination of telmisartan/amlodipine/indapamide compared to 2 drug combinations of these agents demonstrated superior BP control with the triple combination with no difference in withdrawal rates due to adverse events [8]. Similarly, the same triple combination at low doses showed better BP control [goal < 140/90 mmHg (< 18/11 kPa)] compared to standard protocol in a study in Nigeria (82% vs. 72%, respectively) [9]. In addition to the simpler dosing, the synergistic effects of these agents improve their efficacy and utility. The rationale for combining thiazide diuretics and renin angiotensin blockade is based on the natriuresis and volume depletion caused by diuretics leading to activation of the renin angiotensin system (RAS) that is offset by the RAS blockers and further augmented by the vasodilation and sodium/volume reduction caused by RAS blockers leading to better BP control [10]. CCB and RAS blockers are another combination option that are both effective BP lowering agents with complementary mechanisms that target multiple mechanisms involved in vascular disease progression. CCBs not only cause vasodilation by blocking the influx of calcium into vascular smooth muscle cells but also promote fibrinolysis, inhibit proliferation of vascular smooth muscle cells, and inhibit apoptosis of endothelial cells. While RAS blockade triggers vasodilation through blocking the potent vasoconstrictor angiotensin II and a host of positive vascular effects including improving endothelial function as well as vascular inflammation [11]. In addition, combining RAS blockade with CCB appears to minimize the peripheral edema often seen with dihydropyridine CCB treatment [12, 13]. Together these well tolerated long-acting agents are highly effective for treating hypertension.
Fixed dose combination therapy is not without challenges (Table 1). One barrier to the use of combination therapy is the concordance of guideline recommendations. Major hypertension guidelines endorse the use of fixed dose combination therapy as a tactic to improve adherence, particularly in resistant hypertension, however, globally guidelines differ on the strength of the recommendation for fixed dose combination use and the level of BP of initiation of these agents [14]. A second barrier is prescriber reluctance. Several combination therapies are available, yet pharmacy records show that providers do not prescribe fixed dose meds as commonly as single dose meds despite the availability of the same dose strengths [15]. Motivating providers to prescribe fixed dose combination therapy when the proper dosing is available seems like a simpler approach to improve adherence. A recent survey of 191 physicians from 24 countries including 25% working in higher income countries, 38% working in middle income countries, and 6% working in lower income countries assessed opinions regarding factors associated with prescribing fixed dose combination antihypertensives revealed that the most frequently cited barrier in high- and low-income countries is cost and access to these agents. Furthermore, they placed the highest value on using fixed dose combinations in patients with high pill burdens and those who were nonadherent while slightly less on BPs not at goal or high CV risk [16]. A third barrier is cost. Although reducing 2 prescriptions to 1, may seem to logically reduce the cost for patients, this is often not the case. The cost of the fixed dose combination therapy may exceed the cost of 2 separate medications due to the structure of drug pricing and insurance coverage for patients. In a cost-effectiveness analysis in the U.S., the initial single pill antihypertensive options projected per patient medication cost were higher than traditional monotherapy options. However, over time this cost was offset by decreased physician visits, fewer CV events and medication related adverse events. Yet when generic single pill options were available, the initial cost difference favored single pill options [17, 18]. In an analysis of data from the SPRINT trial, 40% of patients in the intensive arm of the study [systolic BP goal was < 120 mmHg (< 15 kPa)] used single pill options, however, only 3.2% of all medication classes used are available as single pill options [19]. Thus availability of combination pill options may be a barrier as well.
Fixed dose combination therapy advantages and challenges
| Advantages | Challenges |
|---|---|
| Decreased pill burdenDecreased co-pay/costIncreased adherenceDecreased clinical inertiaDecreased blood pressureComplementary mechanismsDecreased CVD events | Availability of dose optionsAvailability of drug choice combinationsAccess to fixed dose combinationsCost (inconsistent coverage)Inconsistent guideline recommendations for blood pressure goals and usePrescriber reluctance |
Fixed dose combination drugs for hypertension offer many advantages, although there are a few challenges to consider. CVD: cardiovascular disease
Self-monitoring is widely integrated into guideline therapy for the diagnosis and management of hypertension [20]. Self-monitoring assists with identifying white coat hypertension or white coat effect, masked hypertension, resistant hypertension, and morning hypertension. Providers gain critical knowledge of the pattern of BP elevation and confirmation of the need for additional treatment through accurate home BP assessment. Most self BP assessment programs use traditional arm cuff devices. The addition of self-monitoring is cost effective and efficacious in facilitating medication adherence and better control rates. A 12-week study of hypertensive patients demonstrated an improvement in suboptimal adherence to therapy with the addition of home self BP measurement compared to usual care without home self BP (1.0% compared to 9.9%, P = 0.0005), likewise, BP control improved (66.7% vs. 55.1%, P = 0.04 respectively) [21]. A secondary benefit of home BP assessment is that of reducing clinical inertia by clinicians. Satoh et al. [22] reported that in the Ohasama study, patients reporting home self BP to their physicians were more likely to receive 3 or more classes of BP medications than usual care (41% versus 15% respectively) and achieved better BP control [93.6% versus 43% at the goal of < 135/85 mmHg (< 17/11 kPa)].
While arm cuff BPs are the standard, the use of wrist worn watch devices and other cuffless BP devices may improve adherence through facilitating self-monitoring [23, 24]. Cuffless BP devices are yet another option in out-of-office BP measurement. They range from wrist devices with smartphone applications to wearable ultrasound patches [25]. This technology is early in development in many respects, however, significant progress is being made. Although many of these devices are imperfect in their accuracy, they are useful for following trends. Nevertheless, some emerging devices have shown strong correlation to arterial line measurements [26]. The ease of use and portability of these devices makes them attractive to patients. Surprisingly, wearable devices may also be useful in addressing BP control. Although most wearable fitness devices do not assess BP, individuals who wear fitness devices have higher medication adherence compared to those who do not wear such devices [27]. Thus providing another motivation for greater adherence to medication. In addition, the act of wearing the device may serve as a reminder of their need for hypertension daily treatment.
While BP measurement alone offers clear benefits, the addition of coaching and health messages enhances the effectiveness of home self BP measurement. The widespread use of digital technology facilitates the ability to implement remote coaching. Randomized controlled trials assessing the effect of internet-based interventions of counseling and coaching alone show benefits on BP control, such as a recent trial showing a 4 mmHg (0.5 kPa) decline in clinic systolic BP at 12 months with e-counseling [28]. In the UK, a study of older hypertensive programs that included self-monitoring, dietary advice, dosing adjustments, and behavioral support demonstrated that the HOME and online BP program was more efficacious in achieving BP control compared to usual care (mean decline in BP in intervention group from 151.7/86.4 mmHg (20/11 kPa) to 138.4/80.2 mmHg (18/10 kPa), and in usual care group decline from 151.6/85.3 mmHg (20/11 kPa) to 141.8/79.8 mmHg (18/10 kPa) between intervention group and usual care group [29]). In a similar randomized study of 450 hypertensives, the addition of telephonic nurse management to home BP monitoring improved systolic BP control by 8.1 mmHg (1 kPa) compared to the home BP monitoring group [30]. The same approach is being studied in low- and middle-income countries, in the CONTRACO study using a self-monitoring approach with a treatment algorithm supported by nonphysician health workers in Spain, Colombia, Chile, and Dominican Republic [31]. Such interventions may facilitate better BP control in resource limited communities with less access to healthcare providers.
In addition, the use of smartphones that are integrated with electronic health records can augment adherence and improve control by providing reminders for medicine dosing, as well as making the patient aware of BP level reinforcing the need for medication [32, 33]. Integration of the data directly into the health record may also motivate a stronger relationship with care providers. Thereby promoting titration of doses at earlier intervals for more sustained control [34].
The effectiveness of patient coaching and messaging is best when messaging is adapted to meet the needs of the patient population. Cultural fit, language, and health literacy are essential factors to consider in composing impactful messaging. In a study defining multilevel influences of barriers to BP control, hypertensive African Americans and their family members highlighted the importance of family support in disease management in achieving sustained behavior change [35]. Patterns of eating, exercise, and manners of daily living are clearly determined by the circle of influences on patients. Family and close friendships may affect the behavior of patients around adherence thus counseling messages to patients should consider these aspects of patients’ lives. Furthermore, patient engagement and health literacy impact adherence. Patients with low health literacy also have low adherence to hypertensive medical regimens and other chronic diseases [36, 37]. Thus, providing information that is customized to patients assuring that they understand the material is important. Other novel programs to augment home self BP monitoring programs have included mobilizing lay persons to facilitate patient engagement and knowledge. Trained community health workers, barbers, and health ambassadors are a few examples of successful methods to implement lay persons to enhance proper messaging and improve BP control [38–42]. Community health workers may facilitate communication with communities with limited access to their providers due to distance or cost. A systematic review and meta-analysis of 28 studies of digital health interventions to improve hypertension in vulnerable patient populations found a statistically significant mean reduction in systolic BP of –4.3 mmHg (–0.5 kPa) (P = 0.04) at 12 months compared to usual care. Community health workers were included in 46% of these studies and cultural tailoring was included in 75% of them [43]. Among 6 randomized controlled trials of the effectiveness of community health workers in managing hypertension compared to controls in low-income populations in the U.S., Brownstein et al. [44] reported differences of 4% to 46% in improvement in BP control over 6 to 24 months. Community health workers serve in many roles in these interventions including providing education, increasing access to social services, BP measurement, and mediators to healthcare providers [44]. More recently, community health workers have been shown to be effective components in hypertension management in low- and middle-income countries where the burden of hypertension is rising and access to care is low [45].
The emergence of artificial intelligence (AI) may offer additional benefits to improving adherence. AI techniques for data mining, outcome prediction, assessing BP variability through machine learning clustering, improving self-monitoring devices, as well as assessing adherence patterns and attitudes of patients are augmenting the field to facilitate better BP control [46]. The HOPE Asia Network proposes a practical personalized health record based on the home BP approach that uses time-series big data in digital health and digital medicine to predict the time and place of CV events, described as personalized anticipation medicine [47]. This approach may radically change the face of BP treatment and adherence.
Out-of-office measurement with tailored messaging still faces some challenges with implementation (Table 2). Barriers such as cost of devices and wireless service, ideal messaging that is tailored to patients, and provider workforce time management to handle frequent communication from patients must be considered. While the cost of BP monitors has become more affordable for many, this is not universal. Insurance providers do not universally cover this device. In a survey of hypertensives, 58% responded they had home devices and used them, while of the 23% who did not own a device, 18% reported they could not afford one [48]. Providing free BP cuffs to low-income patients improves BP adherence and control [49]. The observation that wearable devices may affect adherence despite not assessing BP warrants consideration of the cost of these devices. Wearable devices are not cheap, and wide use comes with a cost, however, the return on investment for the escalating risk of uncontrolled hypertension and the human cost makes them more attractive [50, 51]. In the All of Us study of federally qualified health centers, patients with low incomes were less likely to own such devices than patients with higher incomes but they reported that they would wear a fitness device if they were available to them [52].
Self blood pressure monitoring with messaging advantages and challenges
| Advantages | Challenges |
|---|---|
| Facilitates proper diagnosis & managementCost effectiveIncreased adherenceIncreased awarenessDecreases clinical inertiaDecreases blood pressureFacilitates communication with clinicianIncreases health literacyDecreases CVD eventsCommunity health workers offer additional access to support | Proper technique of measurementCalibration of devicesCost of devicesAccess to wireless network servicesAccess to smartphonesComfort with using technology |
Self blood pressure monitoring with messaging offers multiple advantages in the course of treating hypertension, however, some challenges exist to implementation. CVD: cardiovascular disease
Proper use of home devices requires education, and calibration to assure accuracy. Patients can be instructed by staff during clinic visits, however, this requires additional time. Fortunately, many home BP device brands have been validated by international standards and the ratings are freely available at: http://dableducational.org. As more medical clinics are adopting electronic medical records, a larger percentage of patients have become familiar with the use of the portals for enhanced communication with health system providers.
Addressing adherence and the barriers to better BP control requires a thoughtful approach to the unique circumstances of patients. Clinicians should assess the barriers faced by patients to determine the most efficient use of methods to overcome them (Figure 1).
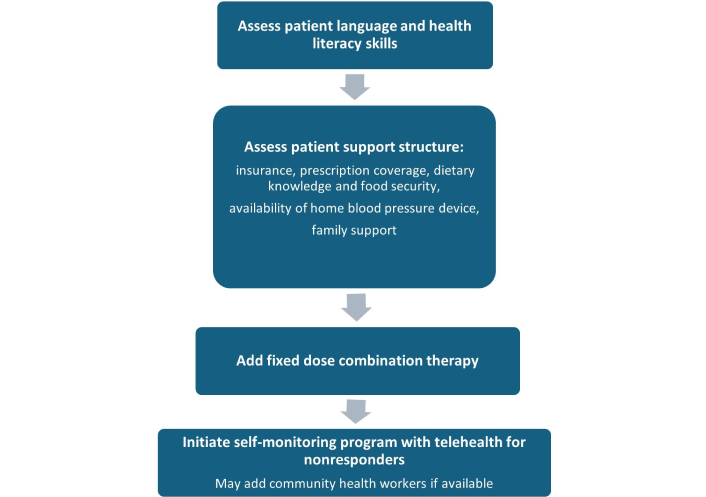
Approach to addressing adherence and barriers to blood pressure control. Selecting an approach for a patient to increase adherence and improve blood pressure should include a stepwise approach to thoughtfully select the best method to achieve success
Closing the gap in hypertension control requires addressing the barriers in a comprehensive manner. A systematic review of barriers to medication adherence in elderly patients identified 80 factors that fit into 5 categories, patient, physician, medication, system based, and other factors [53]. Although this approach was targeted towards elderly patients, it is generalizable to other patient groups. Multifaceted strategies that include fixed dose combination medications, home BP assessment programs with supportive communications are likely to improve not only adherence but most importantly, reduce CV events. Tables 1 and 2 summarize the advantages and challenges of 2 major approaches to reduce nonadherence and enhance BP control. The addition of out-of-office monitoring with patient messaging, particularly with community health workers in low-income populations, will facilitate greater awareness of the lack of BP control, and maintain stronger relationships with health care providers and resources which may help to overcome clinical inertia from providers. Greater access and use of fixed dose combination therapies lead to reduced pill burden and cost for patients, and the complementary mechanisms of fixed dose combination agents enhance effectiveness and mitigate side effects. These 2 approaches are not competitive but rather complement each other to increase adherence and facilitate success in closing the gap in BP control. Clinicians should prioritize the use of these methods, while researchers should concentrate on validating new techniques such as cuffless devices and AI tools for broader application.
AI: artificial intelligence
BP: blood pressure
CCB: calcium channel blocker
CV: cardiovascular
RAS: renin angiotensin system
SDN: Conceptualization, Investigation, Writing—original draft, Writing—review & editing.
I serve as a site co-principal investigator on a study of renal denervation sponsored by Ablative Solutions.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
© The Author(s) 2025.
Open Exploration maintains a neutral stance on jurisdictional claims in published institutional affiliations and maps. All opinions expressed in this article are the personal views of the author(s) and do not represent the stance of the editorial team or the publisher.
Copyright: © The Author(s) 2025. This is an Open Access article licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
View: 1551
Download: 8
Times Cited: 0
Sameen Abbas ... Sohail Kamran
Claudio Tomasino, Marco Tomasino
Eirik Olsen ... Camilla L. Søraas
Vaia Raikou, Sotiris Gavriil
Aaron Walsh ... Ranjit Philip
