Cerebral Ischemia, Genetics, Comorbidities, Risk Factors and New Therapeutic Options for Neurorestoration
Guest Editor
Prof. Aurel Popa-Wagner E-Mail
Chair of Aging and Dementia, NeuroLab, Essen School of Medicine, Germany; Professor of Pathobiochemistry and Experimental Neurology and Director of the Center for Clinical and Experimental Medicine, University of Medicine and Pharmacy, Craiova, Romania.
Research Keywords: Aged animals models of cerebral ischemia, behavioral analysis, recording of EEG and various physiological parameters by telemetric measurements, MRI for small animals, immunohistochemical procedures, proteomics, genomics
About the Special lssue
Globally, cerebrovascular diseases are the second cause of death being surpassed by ischemic heart disease by just 1.5%. Ischemic stroke causes several general and neurological chronic complications, among others physical disability in basic activities of daily living (26%), reduced mobility due to hemiparesis, depression, cognitive decline or dementia and finally, decreased quality of life in different aspects of daily living.
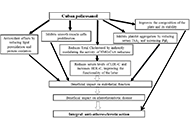
Elderly with a low-risk lifestyle behavior (physical exercise, nonsmoking, healthy nutritious diet, healthy weight during midlife, moderate alcohol consumption) have a significantly lower risk of stroke among women and men than individuals without a low-risk lifestyle. Conversely, elderly with comorbidities including stress, obesity, metabolic syndrome, high cholesterol, diabetes, hypertension, alcoholism, smoking, and a sedentary lifestyle will have a higher incidence of stroke. Clinical data strongly implicate chronic systemic inflammatory conditions, which are associated with metabolic inflammation caused by obesity, atherosclerosis, and hyperlipidemia, in creating a “primed” inflammatory environment in the brain and increasing the vulnerability of the aged brain to stroke and exacerbating poststroke inflammation.
The start of the genome-wide era and the recent progress made in the genetics field have given an approach to find biomarkers and potential drug targets related to poststroke outcomes. Genome-wide association studies (GWAS) are powerful tools to identify genetic variants associated with a trait of interest. These studies allow rapidly scanning markers across the genome of larger population samples interrogating more than hundreds of thousands of genetic variations across the genome.
At tissue level, cerebral ischemia initiates a cascade of molecular and cellular events that has been the subject of intense research in the last several decades. In the first week after cerebral ischemia, proliferating glia become reactive and build up a barrier to regeneration, the glial scar. Direct astroglial reprogramming to neurons using viral vectors carrying transcription factors provides a completely new strategy for neurorestoration after stroke and other traumatic brain injuries.
Although rehabilitation is important for improving functional recovery in the early stages after stroke, it does not provide a replacement of lost tissue. In order to enable the replacement of lost tissue, cell replacement strategies were used in human stroke patients. Most clinical studies conducted so far used neural cells derived from human fetal donors. The techniques to achieve effective survival and growth of neuronal tissues transplanted into the CNS are meanwhile well established. Even though effective, neural grafting has, however, not become a standard treatment for several reasons, including the limited supply of fetal tissue of human origin, and the beneficial effects have been controversial. Of the various options, stem cell therapy presents us with a viable alternative.
In this issue we invite clinicians and scholars of stroke research to contribute to an update of clinical trials and current research cerebral ischemia in an attempt to find new therapeutic options for neurorestoration after insults to the brain.
Keywords: Cerebral ischemia, comorbidities, risk factors, genetic polymorphisms, neurorestoration, glia-to-neurons genetic conversion, new therapeutic approaches
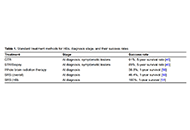
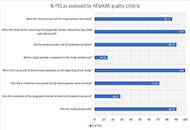
Published Articles